This article at a glance
- The potential utility of the ratio of resolvin D1 (RvD1), a pro-resolving lipid mediator derived from DHA, to leukotriene B4 (LTB4), a pro-inflammatory mediator derived from AA, in saliva was determined to predict the level of non-resolving vascular inflammation.
- The study reports that patients with a higher carotid intima-media thickness as a marker of subclinical atherosclerosis had a significantly lower RvD1/LTB4 ratio.
- The ratio integrates resolution and inflammation processes using lipid mediator levels that can be determined by an ELISA method in readily collected saliva.
- Future studies may validate its use for predicting a range of disorders with unbalanced inflammation, and address the contribution of local oral conditions.
Inflammation is the organ and system response that puts tissues in a state of alert, in order to defend their integrity against infection and physical disruption. However, many non-communicable diseases have a component of unregulated inflammation in their pathology. In a range of inflammatory disorders, the physiological stimuli that trigger the inflammatory response or actively turn inflammation off,
i.e. resolution, are not in a proper balance. The inflammatory response may be unrestrained and too intense, with neutrophils damaging the inflamed tissue, or even triggering a systemic overactivation, with multiple organs being compromised in their function. Or the response may be too long-lasting and chronic, causing a slow process of incremental tissue remodeling and gradual loss of tissue function. The development of atherosclerosis is a good example of a chronically activated inflammatory
response that over the course of many years leads to profound remodeling of sub-endothelial vascular tissue, leading to vascular changes and the formation of hardened plaques that can rupture and form dangerous emboli. A thicker vascular intima is a telltale sign of vascular atheroma formation, which is still at a sub-clinical stage of development, and involves the trans-differentiation of endothelial cells, vascular smooth muscle cells, and stem cells and the net uptake of large amounts of cholesterol by smooth muscle-like
cells and macrophages. Two broad sets of mediators are maintaining a dynamic balance of vascular tissue homeostasis: These include i) pro-inflammatory mediators, which are signalling substances that are formed by the tissue to activate immune cells that normally remove infectious organisms and recruit or activate cells that help repair damaged tissue; and
ii) pro-resolving mediators that limit the extent of the activity of the pro-inflammatory mediators and actively shut down inflammatory responses when metabolic and physical disruption has abated, and there is no more infectious material present anymore, and thus allow and actively promote tissue repair. Atherosclerosis development represents a
chronic maladaptive pro-inflammatory state over the course of years, in response to some forms of continuous stress on the vasculature.
One key pro-inflammatory mediator is leukotriene B
4 (LTB
4), which is produced by macrophages from arachidonic acid (AA) through the activity of the 5-lipoxygenase enzyme, very early in the inflammatory process. LTB
4 promotes the recruitment of additional phagocytes and activates local tissues to produce various cytokines that act in concert to optimize microbial clearance and thus initiate the process for tissue healing. Counteracting the activity of LTB
4 and other pro-inflammatory mediators is important, to limit overactive inflammatory responses that would be destructive to the body’s own tissues. Counter-regulation and active termination of inflammatory responses is executed by pro-resolving mediators that are formed locally during self-limiting inflammation. A
superfamily of pro-resolving molecules formed during self-limiting inflammation is derived from long-chain polyunsaturated fatty acids (LCPUFA), in particular lipoxin A
4 from AA, and resolvins, protectin, maresins and other specialized pro-resolving lipid mediators (SPMs) from the omega-3 LCPUFA, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and docosahexaenoic acid (DHA). Carrying potent inflammation-resolving activity, resolvin D1 (RvD1) is one of the best-characterized SPMs to date. Exposure of macrophages to RvD1 switches their activity towards a less inflammatory
state that is characteristic of a cell type that regulates a variety of processes necessary for orderly resolution. In vascular inflammation, RvD1
reduces the activation of smooth muscle cells by inflammatory stimuli and inhibits the hyperplasia of the intima. In contrast, LTB
4 promotes intimal hyperplasia. A heightened inflammatory response may result from inadequate availability of substrate for SPM formation due to low membrane levels of omega-3 LCPUFA or the reduced expression or activity of the enzymes involved in their biosynthesis. It has been suggested that activating resolution may be a better approach than attempting to only suppress inflammation. Similar indications that the rebalancing of inflammation and its resolution may have significant therapeutic value has recently been drawn for other chronic inflammatory diseases, such as
rheumatoid arthritis.
But how do we know when inflammation resolution needs to be promoted? The levels of lipid mediators in the circulation are generally very low, likely due to rapid metabolic inactivation, and they are very challenging to measure reliably in blood. Measuring these substances within inflamed tissues is often not feasible for internal organs. In a recent study,
Thul and colleagues from the Department of Medicine, Karolinska Institutet in Stockholm, Sweden, in collaboration with researchers from INSERM/University of Lorraine, Nancy, France, and Le Telomere Cardiology Center in Ghardaïa, Algeria, have reported a study that examined the relationship of the RvD1/LTB
4 ratio in saliva with intima-media thickness (IMT).
The researchers made use of samples and data available from 271 participants in the ERA (Etude de la Rigidité Artérielle)
study, a prospective cohort trial carried out in Paris between 1992 and 1999. The
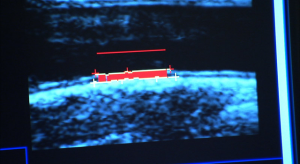
ERA study followed one group of normotensive adults and another group of hypertensive adults that received a free health check covered by the French social security system every five years. The data used in the present report are based on the pooled recorded data at a second visit in 1998-1999, when participants had an average age of ~66 years. IMT of the right common carotid artery was
determined by ultrasound scanning as an indication of subclinical carotid atherosclerosis. Saliva was collected after an overnight fast and prior to performing any oral hygienic interventions (saliva sample storage conditions were not reported). The concentrations of LTB
4 and RvD1 in saliva were determined by enzyme-linked immune assay (ELISA), and could be determined for 254 participants. When these participants were divided into two groups according to their RvD1/LTB
4 ratio ≥1 or <1, a significant difference (P=0.006) in IMT was observed: individuals with RvD1/LTB
4 ≥1 had an average IMT of 0.71 mm, whereas in those with RvD1/LTB
4 <1, mean IMT was 0.76 mm. The 32 individuals (13% of the entire group) with RvD1/LTB
4 ≥1 were not significantly different compared to the other group with respect to gender, average age, blood pressure, heart rate, disease prevalence or pharmacotherapy. However, participants with a ratio ≥1 had a lower body mass index (25.1 compared to 26.6 kg/m
2 (P=0.048; no correction for multiple comparisons was applied)). The median RvD1/LTB
4 ratio in the ratio ≥1 group was 1.37, and 0.28 in the ratio <1 group, showing the separation in ratios (based on median LTB
4 levels of 131 vs 336 pg/ml, and RvD1 levels of 184 vs 97 pg/ml, respectively).
The results of this study show that adults with a high RvD1/LTB
4 ratio in saliva have a significantly lower IMT than people with a low salivary RvD1/LTB
4 ratio. This study suggests that the relative levels of salivary pro-inflammatory and pro-resolving lipid mediators may possibly reflect a systemic or internal organ localized imbalanced inflammatory response, and might be used to stratify people based on their inflammation-resolution balance. Having information from an easily accessible fluid such as saliva may be a helpful additional diagnostic aid in identifying the need for restoring a healthy inflammatory response or the need for turning inflammation off,
potentially using novel future pro-resolving therapeutic approaches. In peripheral atherosclerosis IMT can be measured non-invasively, but the salivary RvD1/LTB
4 ratio may be particularly helpful for assessing inflammation and inflammation-associated pathologies in organ systems that are more challenging to monitor.

Previous studies by these researchers had indicated that salivary C-reactive protein (CRP)
correlates well with systemic circulating CRP levels, a widely used biomarker reflecting inflammation. However, CRP levels are up to 5000-fold more abundant in blood than in saliva. Similar correlations have been obtained for other mediators of inflammation, as well as for metabolic products such as creatinine. Saliva may thus be considered an informative means of monitoring aspects of systemic inflammation and metabolism. For the purpose of using salivary RvD1/LTB
4 ratio as an easily-measurable biomarker of inflammation-resolution balance, it is fortunate, but also surprising, that
saliva contains measurable levels of various lipid mediators, as the levels of many lipid mediator autacoids in the circulation are extremely low. Further studies will need to delineate the origin of RvD1 and LTB
4 in saliva. For example, LTB
4 and RvD1 may be formed within the oral cavity by cells that through yet unclear mechanisms mirror systemic inflammatory status, or they may diffuse from the circulation into the oral cavity where they might be protected from metabolic inactivation. An additional important question, pointed out by the authors, is whether other factors determine the levels of target lipid mediators such as LTB
4 and RvD1 in the oral cavity. For example, does the oral cavity microbiome, dental cleaning frequency, smoking and dietary habits have an influence on these lipid mediator levels in saliva? The development of the RvD1/LTB
4 ratio concept to assess the inflammation-resolution balance for clinical purposes is also an interesting development with respect to currently known read-outs of PUFA status, such as the omega-3 index (which reports the combined abundance of omega-3 LCPUFA as a percentage of total fatty acids in red blood cell membranes), or the ratio of omega-3 to omega-6 LCPUFA abundance in different tissues and fluids. These provide different aspects on the abundance of LCPUFA substrates potentially available for lipid mediator biosynthesis, with higher omega-3 LCPUFA levels correlating well with general health and a propensity for lower intensity inflammatory reactions in chronic or acute disease. In contrast, or complementary to this information, the ratio of the levels of two bioactive lipid mediators with opposing activities in the inflammatory response provides an indication of how AA and DHA, respectively, are transformed by the biosynthetic enzymes involved in their formation plus the net metabolic inactivation up to the time of sampling. It will be interesting to see in future how generally applicable the new RvD1/LTB
4 ratio will be to gauge the state of inflammation in the body, and how it may guide future approaches to inflammation control. Thul S, Labat C, Temmar M, Benetos A, Bäck M. Low salivary resolvin D1 to leukotriene B
4 ratio predicts carotid intima media thickness: A novel biomarker of non-resolving vascular inflammation.
Eur. J. Prev. Cardiol. 2017;24(9):903-906. [
PubMed]
Worth Noting Bäck M, Bu DX, Bränström R, Sheikine Y, Yan ZQ, Hansson GK. Leukotriene B
4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia.
Proc. Natl. Acad. Sci. U.S.A. 2005;102(48):17501-17506. [
PubMed] Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, Thomas F, Pannier B, Asmar R, Zureik M, Safar M, Guize L. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period.
Circulation 2002;105(10):1202-1207. [
PubMed] Dubland JA, Francis GA. So much cholesterol: The unrecognized importance of smooth muscle cells in atherosclerotic foam cell formation.
Curr. Opin. Lipidol. 2016;27(2):155-161. [
PubMed] Elajami TK, Colas RA, Dalli J, Chiang N, Serhan CN, Welty FK. Specialized proresolving lipid mediators in patients with coronary artery disease and their potential for clot remodeling.
FASEB J. 2016;30(8):2792-2801. [
PubMed] Fredman G, Tabas I. Boosting inflammation resolution in atherosclerosis: The next frontier for therapy.
Am. J. Pathol. 2017;187(6):1211-1221. [
PubMed] Labat C, Temmar M, Nagy E, Bean K, Brink C, Benetos A, Bäck M. Inflammatory mediators in saliva associated with arterial stiffness and subclinical atherosclerosis.
J. Hypertens. 2013;31(11):2251-2258. [
PubMed] Miyahara T, Runge S, Chatterjee A, Chen M, Mottola G, Fitzgerald JM, Serhan CN, Conte MS. D-series resolvin attenuates vascular smooth muscle cell activation and neointimal hyperplasia following vascular injury.
FASEB J. 2013;27(6):2220-2232. [
PubMed] Razzak M. Resolving - rather than suppressing - inflammation in RA might be the answer.
Nature Rev Rheumatol 2017;27 July. [
Link] Serhan CN. Treating inflammation and infection in the 21
st century: new hints from decoding resolution mediators and mechanisms.
FASEB J. 2017;31(4):1273-1288. [
PubMed] Simova I. Intima-media thickness: Appropriate evaluation and proper measurement, described.
Electr. J. Cardiol. 2015;13(21). [
Link] Tabas I, Garcia-Cardeña G, Owens GK. Recent insights into the cellular biology of atherosclerosis.
J. Cell Biol. 2015;209(1):13-22. [
PubMed]
 One key pro-inflammatory mediator is leukotriene B4 (LTB4), which is produced by macrophages from arachidonic acid (AA) through the activity of the 5-lipoxygenase enzyme, very early in the inflammatory process. LTB4 promotes the recruitment of additional phagocytes and activates local tissues to produce various cytokines that act in concert to optimize microbial clearance and thus initiate the process for tissue healing. Counteracting the activity of LTB4 and other pro-inflammatory mediators is important, to limit overactive inflammatory responses that would be destructive to the body’s own tissues. Counter-regulation and active termination of inflammatory responses is executed by pro-resolving mediators that are formed locally during self-limiting inflammation. A superfamily of pro-resolving molecules formed during self-limiting inflammation is derived from long-chain polyunsaturated fatty acids (LCPUFA), in particular lipoxin A4 from AA, and resolvins, protectin, maresins and other specialized pro-resolving lipid mediators (SPMs) from the omega-3 LCPUFA, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and docosahexaenoic acid (DHA). Carrying potent inflammation-resolving activity, resolvin D1 (RvD1) is one of the best-characterized SPMs to date. Exposure of macrophages to RvD1 switches their activity towards a less inflammatory state that is characteristic of a cell type that regulates a variety of processes necessary for orderly resolution. In vascular inflammation, RvD1 reduces the activation of smooth muscle cells by inflammatory stimuli and inhibits the hyperplasia of the intima. In contrast, LTB4 promotes intimal hyperplasia. A heightened inflammatory response may result from inadequate availability of substrate for SPM formation due to low membrane levels of omega-3 LCPUFA or the reduced expression or activity of the enzymes involved in their biosynthesis. It has been suggested that activating resolution may be a better approach than attempting to only suppress inflammation. Similar indications that the rebalancing of inflammation and its resolution may have significant therapeutic value has recently been drawn for other chronic inflammatory diseases, such as rheumatoid arthritis.
One key pro-inflammatory mediator is leukotriene B4 (LTB4), which is produced by macrophages from arachidonic acid (AA) through the activity of the 5-lipoxygenase enzyme, very early in the inflammatory process. LTB4 promotes the recruitment of additional phagocytes and activates local tissues to produce various cytokines that act in concert to optimize microbial clearance and thus initiate the process for tissue healing. Counteracting the activity of LTB4 and other pro-inflammatory mediators is important, to limit overactive inflammatory responses that would be destructive to the body’s own tissues. Counter-regulation and active termination of inflammatory responses is executed by pro-resolving mediators that are formed locally during self-limiting inflammation. A superfamily of pro-resolving molecules formed during self-limiting inflammation is derived from long-chain polyunsaturated fatty acids (LCPUFA), in particular lipoxin A4 from AA, and resolvins, protectin, maresins and other specialized pro-resolving lipid mediators (SPMs) from the omega-3 LCPUFA, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA) and docosahexaenoic acid (DHA). Carrying potent inflammation-resolving activity, resolvin D1 (RvD1) is one of the best-characterized SPMs to date. Exposure of macrophages to RvD1 switches their activity towards a less inflammatory state that is characteristic of a cell type that regulates a variety of processes necessary for orderly resolution. In vascular inflammation, RvD1 reduces the activation of smooth muscle cells by inflammatory stimuli and inhibits the hyperplasia of the intima. In contrast, LTB4 promotes intimal hyperplasia. A heightened inflammatory response may result from inadequate availability of substrate for SPM formation due to low membrane levels of omega-3 LCPUFA or the reduced expression or activity of the enzymes involved in their biosynthesis. It has been suggested that activating resolution may be a better approach than attempting to only suppress inflammation. Similar indications that the rebalancing of inflammation and its resolution may have significant therapeutic value has recently been drawn for other chronic inflammatory diseases, such as rheumatoid arthritis.  But how do we know when inflammation resolution needs to be promoted? The levels of lipid mediators in the circulation are generally very low, likely due to rapid metabolic inactivation, and they are very challenging to measure reliably in blood. Measuring these substances within inflamed tissues is often not feasible for internal organs. In a recent study, Thul and colleagues from the Department of Medicine, Karolinska Institutet in Stockholm, Sweden, in collaboration with researchers from INSERM/University of Lorraine, Nancy, France, and Le Telomere Cardiology Center in Ghardaïa, Algeria, have reported a study that examined the relationship of the RvD1/LTB4 ratio in saliva with intima-media thickness (IMT).
But how do we know when inflammation resolution needs to be promoted? The levels of lipid mediators in the circulation are generally very low, likely due to rapid metabolic inactivation, and they are very challenging to measure reliably in blood. Measuring these substances within inflamed tissues is often not feasible for internal organs. In a recent study, Thul and colleagues from the Department of Medicine, Karolinska Institutet in Stockholm, Sweden, in collaboration with researchers from INSERM/University of Lorraine, Nancy, France, and Le Telomere Cardiology Center in Ghardaïa, Algeria, have reported a study that examined the relationship of the RvD1/LTB4 ratio in saliva with intima-media thickness (IMT). 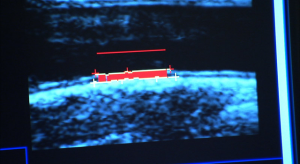 The researchers made use of samples and data available from 271 participants in the ERA (Etude de la Rigidité Artérielle) study, a prospective cohort trial carried out in Paris between 1992 and 1999. The ERA study followed one group of normotensive adults and another group of hypertensive adults that received a free health check covered by the French social security system every five years. The data used in the present report are based on the pooled recorded data at a second visit in 1998-1999, when participants had an average age of ~66 years. IMT of the right common carotid artery was determined by ultrasound scanning as an indication of subclinical carotid atherosclerosis. Saliva was collected after an overnight fast and prior to performing any oral hygienic interventions (saliva sample storage conditions were not reported). The concentrations of LTB4 and RvD1 in saliva were determined by enzyme-linked immune assay (ELISA), and could be determined for 254 participants. When these participants were divided into two groups according to their RvD1/LTB4 ratio ≥1 or <1, a significant difference (P=0.006) in IMT was observed: individuals with RvD1/LTB4 ≥1 had an average IMT of 0.71 mm, whereas in those with RvD1/LTB4 <1, mean IMT was 0.76 mm. The 32 individuals (13% of the entire group) with RvD1/LTB4 ≥1 were not significantly different compared to the other group with respect to gender, average age, blood pressure, heart rate, disease prevalence or pharmacotherapy. However, participants with a ratio ≥1 had a lower body mass index (25.1 compared to 26.6 kg/m2 (P=0.048; no correction for multiple comparisons was applied)). The median RvD1/LTB4 ratio in the ratio ≥1 group was 1.37, and 0.28 in the ratio <1 group, showing the separation in ratios (based on median LTB4 levels of 131 vs 336 pg/ml, and RvD1 levels of 184 vs 97 pg/ml, respectively).
The researchers made use of samples and data available from 271 participants in the ERA (Etude de la Rigidité Artérielle) study, a prospective cohort trial carried out in Paris between 1992 and 1999. The ERA study followed one group of normotensive adults and another group of hypertensive adults that received a free health check covered by the French social security system every five years. The data used in the present report are based on the pooled recorded data at a second visit in 1998-1999, when participants had an average age of ~66 years. IMT of the right common carotid artery was determined by ultrasound scanning as an indication of subclinical carotid atherosclerosis. Saliva was collected after an overnight fast and prior to performing any oral hygienic interventions (saliva sample storage conditions were not reported). The concentrations of LTB4 and RvD1 in saliva were determined by enzyme-linked immune assay (ELISA), and could be determined for 254 participants. When these participants were divided into two groups according to their RvD1/LTB4 ratio ≥1 or <1, a significant difference (P=0.006) in IMT was observed: individuals with RvD1/LTB4 ≥1 had an average IMT of 0.71 mm, whereas in those with RvD1/LTB4 <1, mean IMT was 0.76 mm. The 32 individuals (13% of the entire group) with RvD1/LTB4 ≥1 were not significantly different compared to the other group with respect to gender, average age, blood pressure, heart rate, disease prevalence or pharmacotherapy. However, participants with a ratio ≥1 had a lower body mass index (25.1 compared to 26.6 kg/m2 (P=0.048; no correction for multiple comparisons was applied)). The median RvD1/LTB4 ratio in the ratio ≥1 group was 1.37, and 0.28 in the ratio <1 group, showing the separation in ratios (based on median LTB4 levels of 131 vs 336 pg/ml, and RvD1 levels of 184 vs 97 pg/ml, respectively).  The results of this study show that adults with a high RvD1/LTB4 ratio in saliva have a significantly lower IMT than people with a low salivary RvD1/LTB4 ratio. This study suggests that the relative levels of salivary pro-inflammatory and pro-resolving lipid mediators may possibly reflect a systemic or internal organ localized imbalanced inflammatory response, and might be used to stratify people based on their inflammation-resolution balance. Having information from an easily accessible fluid such as saliva may be a helpful additional diagnostic aid in identifying the need for restoring a healthy inflammatory response or the need for turning inflammation off, potentially using novel future pro-resolving therapeutic approaches. In peripheral atherosclerosis IMT can be measured non-invasively, but the salivary RvD1/LTB4 ratio may be particularly helpful for assessing inflammation and inflammation-associated pathologies in organ systems that are more challenging to monitor.
The results of this study show that adults with a high RvD1/LTB4 ratio in saliva have a significantly lower IMT than people with a low salivary RvD1/LTB4 ratio. This study suggests that the relative levels of salivary pro-inflammatory and pro-resolving lipid mediators may possibly reflect a systemic or internal organ localized imbalanced inflammatory response, and might be used to stratify people based on their inflammation-resolution balance. Having information from an easily accessible fluid such as saliva may be a helpful additional diagnostic aid in identifying the need for restoring a healthy inflammatory response or the need for turning inflammation off, potentially using novel future pro-resolving therapeutic approaches. In peripheral atherosclerosis IMT can be measured non-invasively, but the salivary RvD1/LTB4 ratio may be particularly helpful for assessing inflammation and inflammation-associated pathologies in organ systems that are more challenging to monitor.  Previous studies by these researchers had indicated that salivary C-reactive protein (CRP) correlates well with systemic circulating CRP levels, a widely used biomarker reflecting inflammation. However, CRP levels are up to 5000-fold more abundant in blood than in saliva. Similar correlations have been obtained for other mediators of inflammation, as well as for metabolic products such as creatinine. Saliva may thus be considered an informative means of monitoring aspects of systemic inflammation and metabolism. For the purpose of using salivary RvD1/LTB4 ratio as an easily-measurable biomarker of inflammation-resolution balance, it is fortunate, but also surprising, that saliva contains measurable levels of various lipid mediators, as the levels of many lipid mediator autacoids in the circulation are extremely low. Further studies will need to delineate the origin of RvD1 and LTB4 in saliva. For example, LTB4 and RvD1 may be formed within the oral cavity by cells that through yet unclear mechanisms mirror systemic inflammatory status, or they may diffuse from the circulation into the oral cavity where they might be protected from metabolic inactivation. An additional important question, pointed out by the authors, is whether other factors determine the levels of target lipid mediators such as LTB4 and RvD1 in the oral cavity. For example, does the oral cavity microbiome, dental cleaning frequency, smoking and dietary habits have an influence on these lipid mediator levels in saliva? The development of the RvD1/LTB4 ratio concept to assess the inflammation-resolution balance for clinical purposes is also an interesting development with respect to currently known read-outs of PUFA status, such as the omega-3 index (which reports the combined abundance of omega-3 LCPUFA as a percentage of total fatty acids in red blood cell membranes), or the ratio of omega-3 to omega-6 LCPUFA abundance in different tissues and fluids. These provide different aspects on the abundance of LCPUFA substrates potentially available for lipid mediator biosynthesis, with higher omega-3 LCPUFA levels correlating well with general health and a propensity for lower intensity inflammatory reactions in chronic or acute disease. In contrast, or complementary to this information, the ratio of the levels of two bioactive lipid mediators with opposing activities in the inflammatory response provides an indication of how AA and DHA, respectively, are transformed by the biosynthetic enzymes involved in their formation plus the net metabolic inactivation up to the time of sampling. It will be interesting to see in future how generally applicable the new RvD1/LTB4 ratio will be to gauge the state of inflammation in the body, and how it may guide future approaches to inflammation control. Thul S, Labat C, Temmar M, Benetos A, Bäck M. Low salivary resolvin D1 to leukotriene B4 ratio predicts carotid intima media thickness: A novel biomarker of non-resolving vascular inflammation. Eur. J. Prev. Cardiol. 2017;24(9):903-906. [PubMed] Worth Noting Bäck M, Bu DX, Bränström R, Sheikine Y, Yan ZQ, Hansson GK. Leukotriene B4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia. Proc. Natl. Acad. Sci. U.S.A. 2005;102(48):17501-17506. [PubMed] Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, Thomas F, Pannier B, Asmar R, Zureik M, Safar M, Guize L. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation 2002;105(10):1202-1207. [PubMed] Dubland JA, Francis GA. So much cholesterol: The unrecognized importance of smooth muscle cells in atherosclerotic foam cell formation. Curr. Opin. Lipidol. 2016;27(2):155-161. [PubMed] Elajami TK, Colas RA, Dalli J, Chiang N, Serhan CN, Welty FK. Specialized proresolving lipid mediators in patients with coronary artery disease and their potential for clot remodeling. FASEB J. 2016;30(8):2792-2801. [PubMed] Fredman G, Tabas I. Boosting inflammation resolution in atherosclerosis: The next frontier for therapy. Am. J. Pathol. 2017;187(6):1211-1221. [PubMed] Labat C, Temmar M, Nagy E, Bean K, Brink C, Benetos A, Bäck M. Inflammatory mediators in saliva associated with arterial stiffness and subclinical atherosclerosis. J. Hypertens. 2013;31(11):2251-2258. [PubMed] Miyahara T, Runge S, Chatterjee A, Chen M, Mottola G, Fitzgerald JM, Serhan CN, Conte MS. D-series resolvin attenuates vascular smooth muscle cell activation and neointimal hyperplasia following vascular injury. FASEB J. 2013;27(6):2220-2232. [PubMed] Razzak M. Resolving - rather than suppressing - inflammation in RA might be the answer. Nature Rev Rheumatol 2017;27 July. [Link] Serhan CN. Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J. 2017;31(4):1273-1288. [PubMed] Simova I. Intima-media thickness: Appropriate evaluation and proper measurement, described. Electr. J. Cardiol. 2015;13(21). [Link] Tabas I, Garcia-Cardeña G, Owens GK. Recent insights into the cellular biology of atherosclerosis. J. Cell Biol. 2015;209(1):13-22. [PubMed]
Previous studies by these researchers had indicated that salivary C-reactive protein (CRP) correlates well with systemic circulating CRP levels, a widely used biomarker reflecting inflammation. However, CRP levels are up to 5000-fold more abundant in blood than in saliva. Similar correlations have been obtained for other mediators of inflammation, as well as for metabolic products such as creatinine. Saliva may thus be considered an informative means of monitoring aspects of systemic inflammation and metabolism. For the purpose of using salivary RvD1/LTB4 ratio as an easily-measurable biomarker of inflammation-resolution balance, it is fortunate, but also surprising, that saliva contains measurable levels of various lipid mediators, as the levels of many lipid mediator autacoids in the circulation are extremely low. Further studies will need to delineate the origin of RvD1 and LTB4 in saliva. For example, LTB4 and RvD1 may be formed within the oral cavity by cells that through yet unclear mechanisms mirror systemic inflammatory status, or they may diffuse from the circulation into the oral cavity where they might be protected from metabolic inactivation. An additional important question, pointed out by the authors, is whether other factors determine the levels of target lipid mediators such as LTB4 and RvD1 in the oral cavity. For example, does the oral cavity microbiome, dental cleaning frequency, smoking and dietary habits have an influence on these lipid mediator levels in saliva? The development of the RvD1/LTB4 ratio concept to assess the inflammation-resolution balance for clinical purposes is also an interesting development with respect to currently known read-outs of PUFA status, such as the omega-3 index (which reports the combined abundance of omega-3 LCPUFA as a percentage of total fatty acids in red blood cell membranes), or the ratio of omega-3 to omega-6 LCPUFA abundance in different tissues and fluids. These provide different aspects on the abundance of LCPUFA substrates potentially available for lipid mediator biosynthesis, with higher omega-3 LCPUFA levels correlating well with general health and a propensity for lower intensity inflammatory reactions in chronic or acute disease. In contrast, or complementary to this information, the ratio of the levels of two bioactive lipid mediators with opposing activities in the inflammatory response provides an indication of how AA and DHA, respectively, are transformed by the biosynthetic enzymes involved in their formation plus the net metabolic inactivation up to the time of sampling. It will be interesting to see in future how generally applicable the new RvD1/LTB4 ratio will be to gauge the state of inflammation in the body, and how it may guide future approaches to inflammation control. Thul S, Labat C, Temmar M, Benetos A, Bäck M. Low salivary resolvin D1 to leukotriene B4 ratio predicts carotid intima media thickness: A novel biomarker of non-resolving vascular inflammation. Eur. J. Prev. Cardiol. 2017;24(9):903-906. [PubMed] Worth Noting Bäck M, Bu DX, Bränström R, Sheikine Y, Yan ZQ, Hansson GK. Leukotriene B4 signaling through NF-kappaB-dependent BLT1 receptors on vascular smooth muscle cells in atherosclerosis and intimal hyperplasia. Proc. Natl. Acad. Sci. U.S.A. 2005;102(48):17501-17506. [PubMed] Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, Thomas F, Pannier B, Asmar R, Zureik M, Safar M, Guize L. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation 2002;105(10):1202-1207. [PubMed] Dubland JA, Francis GA. So much cholesterol: The unrecognized importance of smooth muscle cells in atherosclerotic foam cell formation. Curr. Opin. Lipidol. 2016;27(2):155-161. [PubMed] Elajami TK, Colas RA, Dalli J, Chiang N, Serhan CN, Welty FK. Specialized proresolving lipid mediators in patients with coronary artery disease and their potential for clot remodeling. FASEB J. 2016;30(8):2792-2801. [PubMed] Fredman G, Tabas I. Boosting inflammation resolution in atherosclerosis: The next frontier for therapy. Am. J. Pathol. 2017;187(6):1211-1221. [PubMed] Labat C, Temmar M, Nagy E, Bean K, Brink C, Benetos A, Bäck M. Inflammatory mediators in saliva associated with arterial stiffness and subclinical atherosclerosis. J. Hypertens. 2013;31(11):2251-2258. [PubMed] Miyahara T, Runge S, Chatterjee A, Chen M, Mottola G, Fitzgerald JM, Serhan CN, Conte MS. D-series resolvin attenuates vascular smooth muscle cell activation and neointimal hyperplasia following vascular injury. FASEB J. 2013;27(6):2220-2232. [PubMed] Razzak M. Resolving - rather than suppressing - inflammation in RA might be the answer. Nature Rev Rheumatol 2017;27 July. [Link] Serhan CN. Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J. 2017;31(4):1273-1288. [PubMed] Simova I. Intima-media thickness: Appropriate evaluation and proper measurement, described. Electr. J. Cardiol. 2015;13(21). [Link] Tabas I, Garcia-Cardeña G, Owens GK. Recent insights into the cellular biology of atherosclerosis. J. Cell Biol. 2015;209(1):13-22. [PubMed]

