The Relation between Individual Polyunsaturated Fatty Acids and Atherosclerosis Development
This article at a glance
- This prospective multi-ethnic cohort study has examined the relationships between various polyunsaturated fatty acids in plasma phospholipids with the development of atherosclerosis over a 10 year period in adults that were free of cardiovascular disease at baseline.
- The study reports - using vascular imaging techniques - that the level of omega-3 LCPUFA DHA, is negatively correlated with the progression of atherosclerotic vascular lesions. No association with other omega-3 or omega-6 LCPUFA was detected.
- The results support the idea that omega-3 LCPUFA are atheroprotective, but do not support the common notion that linoleic acid is pro-atherogenic.
- Further studies are necessary to strengthen the observed associations, to extend this to specific populations at risk from atherosclerosis, and to determine if these relationships extend to the negative health outcomes of atherosclerosis.
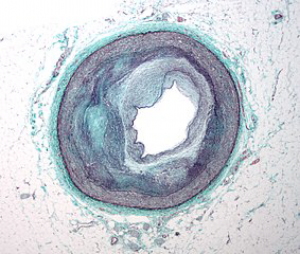
Atherosclerosis is the manifestation of chronic and unresolved vascular damage resulting from localized inflammatory injury to the blood vessel walls, especially those of the arterial vascular system. The development of an atherosclerotic plaque is a relatively slow process that goes through various stages of development, involving the reprogramming of local cell types and defects in the removal of dying cells within the lesion. Initial vascular lesions termed atheromas can progress to hardened and calcified plaques over a period of several years. The clinical consequences and death from atherosclerosis result from the physical rupture of plaques and ensuing formation of life-threatening emboli and thrombi. Cardiovascular diseases are the world’s leading cause of death. Of these, some 80% are caused by heart disease and stroke, for which atherosclerosis is the main responsible mechanism. In the US alone, over 600.000 people die of heart disease every year. Non-fatal infarcts are responsible for a very high incidence of disability. A healthy lifestyle can significantly reduce the risk of development of atherosclerosis and reduce the clinical outcomes of an infarct or stroke.
Food of good nutritional quality can contribute to a healthy lifestyle, but there is still much to be learned about the optimal composition of specific nutrients in our diet. Polyunsaturated fatty acids are one of several important components of food. Since polyunsaturated fatty acids are the biochemical precursors of lipid mediators (enzymatically-oxygenated metabolites of LCPUFA) that are key regulators for the activation and resolution of inflammatory responses, much effort has been made to understand the roles of the various LCPUFA in cardiovascular health. Whereas animal models of atherosclerosis have been very insightful to understand the mechanisms of atherosclerosis etiopathogenesis and can be carried out in relatively short time frames, studies in humans are challenging in that they usually require many years to obtain sufficiently high incidence rates.
Specific for studies on PUFA, such studies are very challenging due to the difficulty of distinguishing the influence and effects of the many fatty acids that each have distinct biological activity. Also, the comprehension of the relative contributions of various polyunsaturated fatty acids to vascular health has for a long time been characterized by a relatively narrow interpretation of their biological roles in the inflammatory process. Thus, omega-6 polyunsaturated fatty acids are seen as pro-inflammatory because arachidonic acid is the precursor to the leukotrienes, prostaglandins and thromboxanes, lipid mediators which have historically been documented as the triggers of inflammation following tissue damage and/or infection. On the other hand, anti-inflammatory activities are attributed to lipid mediators derived from omega-3 LCPUFA, in particular EPA and DHA, and more recently DPA w-3, which limit the extent of the inflammatory responses and drive inflammation to its resolution, when the tissue insult is cleared. Anti-inflammatory and pro-resolving lipid mediators derived from omega-3 LCPUFA comprise several families of substances, including the resolvins, protectins, maresins, and these are added to the 3-series prostaglandins and 5-series leukotrienes.
Although to date no overt inflammation-promoting activities have been attributed to any omega-3 LCPUFA-derived lipid mediators, the converse is not as clear for omega-6 LCPUFA-derived lipid mediators. Some prostaglandins are playing anti-inflammatory and inflammation-resolving roles, e.g. prostaglandin D2 (PGD2) which can function as a pro-resolving lipid mediator in the inflammatory response, and PGE2 which acts as an anti-inflammatory mediator in some organs and conditions. Furthermore, AA-derived lipoxins have inflammation-resolving activities. In other words, a much more nuanced look into the relative and context-dependent roles of polyunsaturated fatty acids needs to be taken when evaluating the importance of the different omega-6 and omega-3 LCPUFA in the many human disorders that include an inflammation component.
Observational and intervention studies support a modest risk reduction in the incidence of cardiovascular disease and mortality, with higher omega-3 intakes. Interestingly, in recent years several studies have also appeared that have provided indications that some but not all omega-6 PUFA may carry or promote pro-inflammatory activity in people, and that their tissue levels are not associated with markers of inflammation or disease outcomes. Whereas a range of methodological issues can be discussed which may affect the strength of outcomes being reported, additional studies that can provide further support for the relationships of individual fatty acids with cardiovascular disease development and the clinical outcomes are needed.
A recent study has explored the association between levels of various LCPUFA in plasma phospholipids at baseline with the progression of atherosclerosis in US American adults, over a period of nearly 10 years. The study was performed by Steffen and colleagues from the Department of Laboratory Medicine and Pathology, at the University of Minnesota, Minneapolis, the University of Minnesota School of Public Health, the Department of Medicine at the University of Wisconsin, Madison, the School of Public Health at the University of Washington, Seattle, the National Institutes of Health Clinical Center, Bethesda, MD, and the Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, U.S.A. The analysis was based on results from the MESA prospective cohort study (Multi-Ethnic Study of Atherosclerosis), which followed 3327 participants over a median period of 9.5 years.
Men and women of age 45-84 years who were free of cardiovascular disease were recruited between 2000-2002. At baseline, several parameters were determined such as age, sex, ethnicity, lifestyle factors, as well as height and weight. Plasma samples were prepared from fasting blood taken at baseline and levels of fatty acids were determined (expressed as percent of the total fatty acid content in the plasma phospholipid fraction). To detect the presence of atherosclerotic plaques in the internal carotid arteries and aorta-carotid artery bifurcations, brightness-mode ultrasonography was conducted at baseline and in 3441 participants at the last of five examinations (in 2010-2012). Certified sonographers aligned the recordings made at both time points. Arterial plaques were scored at a dedicated reading center, and identified as vascular wall thickenings ≥1.5 cm, or focal thickenings at least 50% greater than the surrounding intima media.
At baseline, nearly half of the adults already had atherosclerotic plaques. In this group, a higher proportion of women was present, individuals were older (~5 years on average), more individuals were current or former smokers, and individuals had a higher systolic blood pressure, were more likely to take antihypertensive and lipid-lowering medication and had a higher cholesterol level. In summary, the presence of plaques at baseline was already associated with several typical risk factors for cardiovascular disease. Although the study population was free of cardiovascular disease at baseline, the prevalence of diabetes was twice as high in the group with detectable atherosclerosis (13.6% vs 6.7% in the group without plaques; P<0.001). There was no difference in omega-3 LCPUFA levels between individuals with or without plaques (EPA plus DHA levels were approximately 4.8%), but linoleic acid levels were a bit lower in the group with plaques (19.96% vs 20.50% in the group without plaques; P<0.001).
Of the 3296 individuals who were reassessed 9.5 years later, 1854 (56 %) showed a progression of carotid plaque development. The absence of plaque progression was characterized by the same characteristics as found in individuals without arterial plaques; having a lower age, a lower proportion of women, a lower proportion of current and former smokers, lower BMI, lower systolic blood pressure, lower use of blood pressure and lipid-lowering medication, fewer diabetics, and a small but significantly higher level of linoleic acid. The only difference in the group of people that displayed no progression in atherosclerosis development was a small but statistically significantly higher level of DHA in plasma phospholipids (3.97% vs 3.82% in the group where atherosclerosis progressed). No changes in other LCPUFA, such as EPA or AA, were associated with absence of atherosclerosis development.
Given the suggested associations of LA and DHA with a possible reduced risk of plaque progression during the 10-year follow-up, the researchers examined whether higher levels of these fatty acids were related to a lower relative risk of plaque at baseline, as well as for atherosclerosis progression. Individuals with the highest quartile of DHA levels had a 9% lower risk of having carotid plaques at baseline. No relation between LA levels and plaque presence at baseline was detected. For plaque progression, a reduction in risk was found in the three highest quartiles of DHA, with a statistically significant 12% decrease (P<0.01) in the highest quartile, but there was no relation between LA levels (as quartiles) and relative risk of plaque progression. All associations were tested after adjustments for age, sex, race/ethnicity, BMI, hypertension, medication use, smoking, blood pressure, diabetes, and cholesterol.
Given the relatively small changes in risk associated with DHA at baseline and plaque progression, the results should be interpreted with caution. In fact, alpha-linolenic acid (ALA) levels in the second quartile only were associated with an 11% increase in risk of plaque presence at baseline, which from the point of assuming a linear dose-response (if ALA would influence vascular inflammation) does not make sense. The results of this study should hence be viewed as informative for further research.
This study confirms that atherosclerosis development can be attenuated in a significant proportion of adults of multi-ethnic origins and is associated with a lower incidence of several well-known modifiable risk factors for cardiovascular disease. The study also provides indications that a higher DHA status may lower the risk for atherosclerosis development, although plasma phospholipids do not seem to be a lipid pool where changes in tissue status of DHA can be detected in a sensitive manner. The result support the known vasculo-protective activity of omega-3 LCPUFA intake. Perhaps more interesting is the observation that an increased blood level of linoleic acid was not associated with increased atherosclerosis. This notion challenges oversimplified views that assign a pro-inflammatory effect to higher levels of omega-6 fatty acids. To confirm that there is no relation between LA and vascular inflammation, more precise measurements of fatty acid levels should ideally be made within the vascular tissue and the immune cells within inflamed vascular lesions (atheromas and sclerosing plaques). Such measurements are however difficult to make in people.
Remarkably, the risk of death from ischemic heart disease was recently reported to be negatively related to serum levels of linoleic acid. In a prospective cohort study of 2840 adult Finnish men, over a 24-year period, individuals in the highest quartile of serum linoleic acid had a 46% reduced risk of death from cardiovascular disease compared to men with the lowest levels. These men were 42-60-years old at baseline, a portion of which likely already had developed some degree of atherosclerosis, and which further progressed during the long follow-up. These results suggest that higher linoleic acid levels are not necessarily prejudicial for cardiovascular health in a broad sense, and may even be protective when atherosclerotic plaques have already developed.
Is it possible that linoleic acid does not contribute to the development of atherosclerosis, but that higher linoleic acid offers protection against the lethal outcomes of ischemic disorders resulting from advanced atherosclerosis? That conclusion cannot be drawn from observational research. To better understand the relationships between individual LCPUFA it is likely that much greater detail needs to be paid to the precise stage of atherosclerosis and cardiovascular disease development, and the clinical outcomes that are reported. It is probable that the tissue level of omega-3 LCPUFA needs to be sufficiently high to provide a certain degree of inflammation-lowering potential, as shown for the association of DHA with reducing aortic lesion development and progression. Although there were no associations of EPA with plaque progression in these studies, EPA is incorporated into arterial plaques in humans. Such plaques have less inflammation and have thicker fibrous caps. This plaque-stabilizing activity reduces the risk of plaque rupture and subsequent thrombotic sequelae. In light of the results of the two prospective studies highlighted here, in combination with the growing appreciation for stage-specific activity of individual LCPUFA species, new studies that evaluate the molecular mechanisms of a potential protective activity of linoleic acid in advanced atherosclerosis and ischemic outcomes could be informative. Unlike for long-chain omega-3 LCPUFA, higher LA intakes have previously been reported not to affect plaque stability. Further research is still necessary to disentangle the seemingly confusing functions that individual fatty acids have in regulating cardiovascular health.
Steffen BT, Guan W, Stein JH, Tattersall MC, Kaufman JD, Sandfort V, Szklo M, Tsai MY. Plasma n-3 and n-6 fatty acids are differentially related to carotid plaque and its progression: The Multi-Ethnic Study of Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2018;38(3):653-659. [PubMed]
Virtanen JK, Wu JHY, Voutilainen S, Mursu J, Tuomainen TP. Serum n-6 polyunsaturated fatty acids and risk of death: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am. J. Clin. Nutr. 2018;107(3):427-435. [PubMed]
Worth Noting
Alexander DD, Miller PE, Van Elswyk ME, Kuratko CN, Bylsma LC. A meta-analysis of randomized controlled trials and prospective cohort studies of eicosapentaenoic and docosahexaenoic long-chain omega-3 fatty acids and coronary heart disease risk. Mayo Clin. Proc. 2017;92(1):15-29. [PubMed]
Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr., Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am. J. Epidemiol. 2002;156(9):871-881. [PubMed]
B-mode ultrasonography : Link
Cawood AL, Ding R, Napper FL, Young RH, Williams JA, Ward MJ, Gudmundsen O, Vige R, Payne SP, Ye S, Shearman CP, Gallagher PJ, Grimble RF, Calder PC. Eicosapentaenoic acid (EPA) from highly concentrated n-3 fatty acid ethyl esters is incorporated into advanced atherosclerotic plaques and higher plaque EPA is associated with decreased plaque inflammation and increased stability. Atherosclerosis 2010;212(1):252-259. [PubMed]
Centers for Disease Control - Heart Disease Facts: https://www.cdc.gov/heartdisease/facts.htm
Centers for Disease Control – Healthy Living: https://www.cdc.gov/stroke/healthy_living.htm
Delgado GE, März W, Lorkowski S, von Schacky C, Kleber ME. Omega-6 fatty acids: Opposing associations with risk-The Ludwigshafen Risk and Cardiovascular Health Study. J. Clin. Lipidol. 2017;11(4):1082-1090. [PubMed]
Innes JK, Calder PC. Omega-6 fatty acids and inflammation. Prostaglandins Leukot. Essent. Fatty Acids 2018;132:41-48. [PubMed]
Thies F, Garry JM, Yaqoob P, Rerkasem K, Williams J, Shearman CP, Gallagher PJ, Calder PC, Grimble RF. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet 2003;361(9356):477-485. [PubMed]
World Health Organization – Cardiovascular Disease: http://www.who.int/cardiovascular_diseases/en/
Yurdagul AJ, Doran AC, Cai B, Fredman G, Tabas IA. Mechanisms and consequences of defective efferocytosis in atherosclerosis. Front. Cardiovasc. Med. 2018;4(86). [PubMed]

