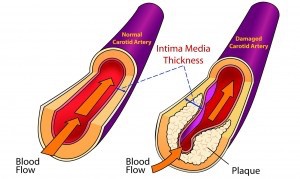
In the preceding article, EPA was associated with a lower risk of heart failure, but DHA was not. These are the main two long-chain omega-3 fatty acids (omega-3s) found in seafood and both contribute to a lower risk of heart disease. It is likely, however, that they may operate differently, yet still be complementary in protecting heart health. In this article, we describe a study among Japanese and US men in which high levels of DHA, but not EPA, were associated with a more favorable marker of atherosclerosis, the thickness of the carotid artery wall. Measuring the arterial wall in this neck artery is readily done using ultrasound techniques and provides the physician with an indication of the extent of a patient’s atherosclerosis. When assessed over time, this measurement—carotid intima-media thickness—abbreviated as CIMT, allows the physician to monitor the progression or regression of atherosclerotic disease (Figure). CIMT is also an independent predictor of coronary artery disease and because it is non-invasive is used by many cardiologists.
Long-chain omega-3s have been associated with lower CIMT measures and with a slower progression (or even regression) of atherosclerosis observed in the coronary arteries. There has also been a report from Spain that CIMT scores were lower in adults who had higher DHA levels in their blood. There is little evidence to suggest that EPA and DHA might have different effects on CIMT. A new study looked at samples of middle-aged men with elevated heart disease risk factors selected from populations in Japan andthe U.S. The Japanese participants had higher rates of smoking, hypertension and diabetes, but were less likely to be overweight and ate much more fish. The US men were more likely to exercise. Thus, both groups had some lifestyle factors working for and against their heart health.
The differences in fish consumption appeared in the blood levels of EPA, DHA and total long-chain omega-3s. The median level for total omega-3s in Japanese was 8.8% compared with 3.5% for the US men. In both groups, the DHA concentration in blood was related to lower CIMT scores, but EPA was not. However, when the investigators took into account other confounding variables besides age, higher blood DHA was associated with lower CIMT scores only in the Japanese men, not the US group. These findings support those of a previously reported Spanish study and suggest that higher levels of DHA, but not EPA, are related to lower CIMT scores. The study does not explain why the CIMT scores in one set of men were related to DHA, but not in the other. Was it the fact that US men had less than half as much DHA as their Japanese counterparts? That could be a possible explanation. This study is an observational report and does not tell us whether the association between DHA and CIMT is causal. As both DHA and EPA are often found together in foods containing long-chain omega-3s, such as fish, egg yolk and many fish oil supplements, the study may be of greatest interest to physicians and researchers. The findings add to the substantial literature documenting diverse protective effects of long-chain omega-3s in heart health.
 In the preceding article, EPA was associated with a lower risk of heart failure, but DHA was not. These are the main two long-chain omega-3 fatty acids (omega-3s) found in seafood and both contribute to a lower risk of heart disease. It is likely, however, that they may operate differently, yet still be complementary in protecting heart health. In this article, we describe a study among Japanese and US men in which high levels of DHA, but not EPA, were associated with a more favorable marker of atherosclerosis, the thickness of the carotid artery wall. Measuring the arterial wall in this neck artery is readily done using ultrasound techniques and provides the physician with an indication of the extent of a patient’s atherosclerosis. When assessed over time, this measurement—carotid intima-media thickness—abbreviated as CIMT, allows the physician to monitor the progression or regression of atherosclerotic disease (Figure). CIMT is also an independent predictor of coronary artery disease and because it is non-invasive is used by many cardiologists.
In the preceding article, EPA was associated with a lower risk of heart failure, but DHA was not. These are the main two long-chain omega-3 fatty acids (omega-3s) found in seafood and both contribute to a lower risk of heart disease. It is likely, however, that they may operate differently, yet still be complementary in protecting heart health. In this article, we describe a study among Japanese and US men in which high levels of DHA, but not EPA, were associated with a more favorable marker of atherosclerosis, the thickness of the carotid artery wall. Measuring the arterial wall in this neck artery is readily done using ultrasound techniques and provides the physician with an indication of the extent of a patient’s atherosclerosis. When assessed over time, this measurement—carotid intima-media thickness—abbreviated as CIMT, allows the physician to monitor the progression or regression of atherosclerotic disease (Figure). CIMT is also an independent predictor of coronary artery disease and because it is non-invasive is used by many cardiologists.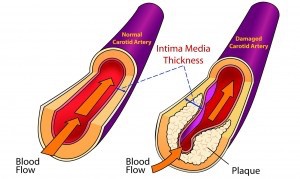 Long-chain omega-3s have been associated with lower CIMT measures and with a slower progression (or even regression) of atherosclerosis observed in the coronary arteries. There has also been a report from Spain that CIMT scores were lower in adults who had higher DHA levels in their blood. There is little evidence to suggest that EPA and DHA might have different effects on CIMT. A new study looked at samples of middle-aged men with elevated heart disease risk factors selected from populations in Japan andthe U.S. The Japanese participants had higher rates of smoking, hypertension and diabetes, but were less likely to be overweight and ate much more fish. The US men were more likely to exercise. Thus, both groups had some lifestyle factors working for and against their heart health.
Long-chain omega-3s have been associated with lower CIMT measures and with a slower progression (or even regression) of atherosclerosis observed in the coronary arteries. There has also been a report from Spain that CIMT scores were lower in adults who had higher DHA levels in their blood. There is little evidence to suggest that EPA and DHA might have different effects on CIMT. A new study looked at samples of middle-aged men with elevated heart disease risk factors selected from populations in Japan andthe U.S. The Japanese participants had higher rates of smoking, hypertension and diabetes, but were less likely to be overweight and ate much more fish. The US men were more likely to exercise. Thus, both groups had some lifestyle factors working for and against their heart health.  The differences in fish consumption appeared in the blood levels of EPA, DHA and total long-chain omega-3s. The median level for total omega-3s in Japanese was 8.8% compared with 3.5% for the US men. In both groups, the DHA concentration in blood was related to lower CIMT scores, but EPA was not. However, when the investigators took into account other confounding variables besides age, higher blood DHA was associated with lower CIMT scores only in the Japanese men, not the US group. These findings support those of a previously reported Spanish study and suggest that higher levels of DHA, but not EPA, are related to lower CIMT scores. The study does not explain why the CIMT scores in one set of men were related to DHA, but not in the other. Was it the fact that US men had less than half as much DHA as their Japanese counterparts? That could be a possible explanation. This study is an observational report and does not tell us whether the association between DHA and CIMT is causal. As both DHA and EPA are often found together in foods containing long-chain omega-3s, such as fish, egg yolk and many fish oil supplements, the study may be of greatest interest to physicians and researchers. The findings add to the substantial literature documenting diverse protective effects of long-chain omega-3s in heart health.
The differences in fish consumption appeared in the blood levels of EPA, DHA and total long-chain omega-3s. The median level for total omega-3s in Japanese was 8.8% compared with 3.5% for the US men. In both groups, the DHA concentration in blood was related to lower CIMT scores, but EPA was not. However, when the investigators took into account other confounding variables besides age, higher blood DHA was associated with lower CIMT scores only in the Japanese men, not the US group. These findings support those of a previously reported Spanish study and suggest that higher levels of DHA, but not EPA, are related to lower CIMT scores. The study does not explain why the CIMT scores in one set of men were related to DHA, but not in the other. Was it the fact that US men had less than half as much DHA as their Japanese counterparts? That could be a possible explanation. This study is an observational report and does not tell us whether the association between DHA and CIMT is causal. As both DHA and EPA are often found together in foods containing long-chain omega-3s, such as fish, egg yolk and many fish oil supplements, the study may be of greatest interest to physicians and researchers. The findings add to the substantial literature documenting diverse protective effects of long-chain omega-3s in heart health.

