Dry eye syndrome is a condition of reduced quantity or quality of tears that increases the risk of ocular surface infections and has bothersome symptoms that interfere with activities such as reading, working at a computer and driving a car. Individuals who develop the condition are
more likely to be female, older, have reduced androgen levels, use exogenous estrogen, have imbalanced intakes of PUFAs and take certain medications. Data from two large prospective, U.S. studies in health professionals reported that 3.3 million women and 1.7 million men aged 50 and older have symptoms of dry eye. The
American Optometric Association reports that the majority of people over the age of 65 experience some symptom of dry eyes. Underlying dry eye is frequently a dysfunction of the
meibomian glands, specialized sebaceous glands that lie in the thick connective tissue layer of the eyelid rims. They produce a lipid secretion—meibum—that prevents the rapid evaporation and spillage of tear fluid and makes the closed eyelids tight. Disorders of these glands include blockage, thickening of the meibum and inflammation that lead to tear deficiency and instability and a shortening of tear breakup time (Figure 1).

Several studies have explored the involvement of long-chain PUFAs (LC-PUFA), especially n-3 LC-PUFAs in
alleviating the symptoms of dry eye, promoting
corneal nerve regeneration after surgery and
reducing markers of inflammation. In addition, the topical application of
alpha-linolenic acid was associated with a significant decrease in dry eye symptoms. The relationship between the dietary consumption of n-3 PUFAs or both n-3 and n-6 PUFAs and the incidence of dry eye was
first reported in 2005 for data from the Women’s Health Study. Women with the highest intakes of DHA or tuna experienced a significantly lower risk of dry eye compared with women in the lowest intake categories.
Improvements in dry eye symptoms with supplements of n-3 and n-6 PUFAs were observed shortly thereafter. Although dietary studies with PUFAs have increased, few have examined the effectiveness of dietary n-3 LC-PUFAs without n-6 PUFAs in conditions of meibomian gland dysfunction. A new study from Spain evaluated the effectiveness of 3 months’ supplementation with DHA-rich n-3 LC-PUFAs plus antioxidant vitamins and minerals in improving the objective signs and clinical symptoms of meibomian gland dysfunction. The primary outcomes were fluorescein corneal staining and tear breakup time, with secondary outcomes the Schirmer I test for tear quantity and dry eye symptoms. Sixty-four patients with clinically diagnosed meibomian gland dysfunction were recruited from the University Hospital Jiménez Díaz Foundation, Madrid, Spain. Participants were 56 years of age on average and were free from systemic diseases, ophthalmic laser treatment within the past 3 months, blepharitis (inflammation of the eyelids) without meibomian gland dysfunction, ocular disorders and eye drops other than artificial tears. Prior to the baseline visit, participants were required to discontinue using nutritional supplements, antibiotics, non-steroidal anti-inflammatory drugs, corticosteroids and artificial tears containing vitamins for at least 15 days. Ocular lubricants without nutrients were permitted. Patients were enrolled according to the
diagnostic criteria for meibomian gland dysfunction established by an international working group. Meibomian gland dysfunction was classified according to the nature of the abnormal discharge or anomalous expression in response to a finger placed on both eyelids.
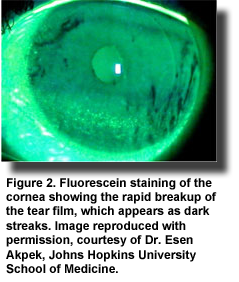
At baseline, tear breakup time was measured by the disappearance time for one fluorescein drop and corneal fluorescein staining (Figure 2) was graded according to the Oxford Test as described by the Diagnostic Subcommittee of the
International Dry Eye Workshop. The investigators quantified tear production by the
Schirmer I test without anesthesia, assessed disease severity using the
Ocular Surface Disease Index questionnaire and clinically evaluated the quality of the meibomian secretion, lid margin inflammation and corneal dye staining. All participants applied a warm compress to the eyes for 5 minutes daily. In this double-blind stu
dy, participants were randomly assigned to consume 3 capsules daily, one per meal, of the n-3 LC-PUFAs plus antioxidants or a sunflower oil placebo without antioxidants. The total dose of n-3 LC-PUFAs per day was 1.3 g, providing 1.05 g of DHA, 128 mg of EPA and 30 mg DPA. Other capsule constituents included vitamins A, C, E, tyrosine, cysteine, glutathione, zinc, copper, manganese and selenium. Supplementation continued for 3 months, with objective assessments taken at monthly participant visits after baseline. Sixty-one participants completed the study.
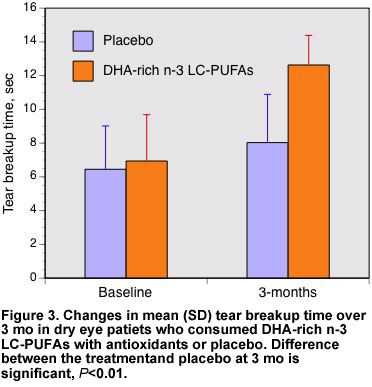
After 3 months, the tear breakup time was significantly increased in the n-3 LC-PUFA-supplemented participants with no significant change in the placebo group (Figure 3). Increased breakup time indicates a more stable tear film. Significant improvements compared with the control group were apparent at each monthly assessment. Cornea staining and tear quantity did not differ between the groups or from baseline values. Other significant improvements with n-3 LC-PUFA supplementation included decreased lid inflammation compared with baseline and increased meibomian gland expressibility. Both groups experienced significant decreases in the severity of their symptoms, such as sensitivity to light, soreness and a gritty feeling in the eyes. The study did not control for the antioxidants consumed with the n-3 LC-PUFA supplement, so the results cannot entirely be attributed to the effect of the n-3 PUFAs. However, the results are consistent with other findings in dry eye studies attributable to n-3 LC-PUFAs. This study demonstrated that 3 months’ consumption of a moderately high dose of DHA-rich n-3 LC-PUFAs was associated with a significant improvement in tear stability, reduction in eyelid inflammation and decreased clinical symptoms of meibomian gland dysfunction. These findings are consistent with the increased tear production observed in mice with dry eye treated with
resolvin E1, a derivative of EPA; with clinical improvements in patients with keratoconjunctivitis sicca who consumed
n-3 PUFAs and gamma-linolenic acid for 6 months; and with significant improvements in a short-term
clinical study of patients with dry eye who consumed 600 mg/day of n-3 LC-PUFAs.
One can speculate that the anti-inflammatory effects of n-3 LC-PUFAs contributed to the observed clinical improvements, but other than reduced eyelid inflammation and clinical symptoms, no objective measures of inflammatory markers were performed. However, the anti-inflammatory effects of this supplement were described in a
similar study using a lower dose of the same preparation. The investigators reported significantly improved clinical symptoms and significantly lower tear levels of IL-1β, ΙL-6 and IL-10 after 3 months’ supplementation with the DHA-rich n-3 LC-PUFAs and antioxidants. The present study provides a clear demonstration that DHA-rich n-3 LC-PUFA supplementation improves clinical and objective measures of meibomian gland dysfunction as observed in patients with dry eye syndrome. Even though the literature is not extensive, it has become common for
optometrists,
clinics and patient
education materials to suggest increased consumption of omega-3 PUFAs for patients with dry eye disease. More good reasons to do so are emerging. Oleñik A, Jiménez-Alfaro I, Alejandre-Alba N, Mahillo-Fernández I. A randomized, double-masked study to evaluate the effect of omega-3 fatty acids supplementation in meibomian gland dysfunction.
Clin Interv Aging 2013;8:1133-1138. [
PubMed] Open Access
Worth Noting Sheppard JD Jr, Singh R, McClellan AJ, Weikert MP, Scoper SV, Joly TJ, Whitley WO, Kakkar E, Pflugfelder SC. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: A randomized double-blind clinical trial.
Cornea 2013; Jul 23. [Epub ahead of print] [
PubMed] Kangari H, Eftekhari MH, Sardari S, Hashemi H, Salamzadeh J, Ghassemi-Broumand M, Khabazkhoob M. Short-term consumption of oral omega-3 and dry eye syndrome.
Ophthalmology 2013;120:2191-2196. [
PubMed] Kenchegowda S, He J, Bazan HE. Involvement of pigment epithelium-derived factor, docosahexaenoic acid and neuroprotectin D1 in corneal inflammation and nerve integrity after refractive surgery.
Prostaglandins Leukot Essent Fatty Acids 2013;88:27-31. [
PubMed] Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction.
PLoS One 2013;8:e76121. [
PubMed] Open Access
 Dry eye syndrome is a condition of reduced quantity or quality of tears that increases the risk of ocular surface infections and has bothersome symptoms that interfere with activities such as reading, working at a computer and driving a car. Individuals who develop the condition are more likely to be female, older, have reduced androgen levels, use exogenous estrogen, have imbalanced intakes of PUFAs and take certain medications. Data from two large prospective, U.S. studies in health professionals reported that 3.3 million women and 1.7 million men aged 50 and older have symptoms of dry eye. The American Optometric Association reports that the majority of people over the age of 65 experience some symptom of dry eyes. Underlying dry eye is frequently a dysfunction of the meibomian glands, specialized sebaceous glands that lie in the thick connective tissue layer of the eyelid rims. They produce a lipid secretion—meibum—that prevents the rapid evaporation and spillage of tear fluid and makes the closed eyelids tight. Disorders of these glands include blockage, thickening of the meibum and inflammation that lead to tear deficiency and instability and a shortening of tear breakup time (Figure 1).
Dry eye syndrome is a condition of reduced quantity or quality of tears that increases the risk of ocular surface infections and has bothersome symptoms that interfere with activities such as reading, working at a computer and driving a car. Individuals who develop the condition are more likely to be female, older, have reduced androgen levels, use exogenous estrogen, have imbalanced intakes of PUFAs and take certain medications. Data from two large prospective, U.S. studies in health professionals reported that 3.3 million women and 1.7 million men aged 50 and older have symptoms of dry eye. The American Optometric Association reports that the majority of people over the age of 65 experience some symptom of dry eyes. Underlying dry eye is frequently a dysfunction of the meibomian glands, specialized sebaceous glands that lie in the thick connective tissue layer of the eyelid rims. They produce a lipid secretion—meibum—that prevents the rapid evaporation and spillage of tear fluid and makes the closed eyelids tight. Disorders of these glands include blockage, thickening of the meibum and inflammation that lead to tear deficiency and instability and a shortening of tear breakup time (Figure 1).  Several studies have explored the involvement of long-chain PUFAs (LC-PUFA), especially n-3 LC-PUFAs in alleviating the symptoms of dry eye, promoting corneal nerve regeneration after surgery and reducing markers of inflammation. In addition, the topical application of alpha-linolenic acid was associated with a significant decrease in dry eye symptoms. The relationship between the dietary consumption of n-3 PUFAs or both n-3 and n-6 PUFAs and the incidence of dry eye was first reported in 2005 for data from the Women’s Health Study. Women with the highest intakes of DHA or tuna experienced a significantly lower risk of dry eye compared with women in the lowest intake categories. Improvements in dry eye symptoms with supplements of n-3 and n-6 PUFAs were observed shortly thereafter. Although dietary studies with PUFAs have increased, few have examined the effectiveness of dietary n-3 LC-PUFAs without n-6 PUFAs in conditions of meibomian gland dysfunction. A new study from Spain evaluated the effectiveness of 3 months’ supplementation with DHA-rich n-3 LC-PUFAs plus antioxidant vitamins and minerals in improving the objective signs and clinical symptoms of meibomian gland dysfunction. The primary outcomes were fluorescein corneal staining and tear breakup time, with secondary outcomes the Schirmer I test for tear quantity and dry eye symptoms. Sixty-four patients with clinically diagnosed meibomian gland dysfunction were recruited from the University Hospital Jiménez Díaz Foundation, Madrid, Spain. Participants were 56 years of age on average and were free from systemic diseases, ophthalmic laser treatment within the past 3 months, blepharitis (inflammation of the eyelids) without meibomian gland dysfunction, ocular disorders and eye drops other than artificial tears. Prior to the baseline visit, participants were required to discontinue using nutritional supplements, antibiotics, non-steroidal anti-inflammatory drugs, corticosteroids and artificial tears containing vitamins for at least 15 days. Ocular lubricants without nutrients were permitted. Patients were enrolled according to the diagnostic criteria for meibomian gland dysfunction established by an international working group. Meibomian gland dysfunction was classified according to the nature of the abnormal discharge or anomalous expression in response to a finger placed on both eyelids.
Several studies have explored the involvement of long-chain PUFAs (LC-PUFA), especially n-3 LC-PUFAs in alleviating the symptoms of dry eye, promoting corneal nerve regeneration after surgery and reducing markers of inflammation. In addition, the topical application of alpha-linolenic acid was associated with a significant decrease in dry eye symptoms. The relationship between the dietary consumption of n-3 PUFAs or both n-3 and n-6 PUFAs and the incidence of dry eye was first reported in 2005 for data from the Women’s Health Study. Women with the highest intakes of DHA or tuna experienced a significantly lower risk of dry eye compared with women in the lowest intake categories. Improvements in dry eye symptoms with supplements of n-3 and n-6 PUFAs were observed shortly thereafter. Although dietary studies with PUFAs have increased, few have examined the effectiveness of dietary n-3 LC-PUFAs without n-6 PUFAs in conditions of meibomian gland dysfunction. A new study from Spain evaluated the effectiveness of 3 months’ supplementation with DHA-rich n-3 LC-PUFAs plus antioxidant vitamins and minerals in improving the objective signs and clinical symptoms of meibomian gland dysfunction. The primary outcomes were fluorescein corneal staining and tear breakup time, with secondary outcomes the Schirmer I test for tear quantity and dry eye symptoms. Sixty-four patients with clinically diagnosed meibomian gland dysfunction were recruited from the University Hospital Jiménez Díaz Foundation, Madrid, Spain. Participants were 56 years of age on average and were free from systemic diseases, ophthalmic laser treatment within the past 3 months, blepharitis (inflammation of the eyelids) without meibomian gland dysfunction, ocular disorders and eye drops other than artificial tears. Prior to the baseline visit, participants were required to discontinue using nutritional supplements, antibiotics, non-steroidal anti-inflammatory drugs, corticosteroids and artificial tears containing vitamins for at least 15 days. Ocular lubricants without nutrients were permitted. Patients were enrolled according to the diagnostic criteria for meibomian gland dysfunction established by an international working group. Meibomian gland dysfunction was classified according to the nature of the abnormal discharge or anomalous expression in response to a finger placed on both eyelids. 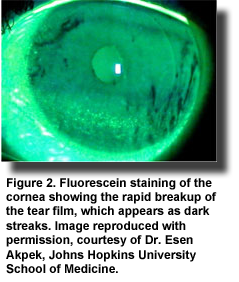 At baseline, tear breakup time was measured by the disappearance time for one fluorescein drop and corneal fluorescein staining (Figure 2) was graded according to the Oxford Test as described by the Diagnostic Subcommittee of the International Dry Eye Workshop. The investigators quantified tear production by the Schirmer I test without anesthesia, assessed disease severity using the Ocular Surface Disease Index questionnaire and clinically evaluated the quality of the meibomian secretion, lid margin inflammation and corneal dye staining. All participants applied a warm compress to the eyes for 5 minutes daily. In this double-blind stu
At baseline, tear breakup time was measured by the disappearance time for one fluorescein drop and corneal fluorescein staining (Figure 2) was graded according to the Oxford Test as described by the Diagnostic Subcommittee of the International Dry Eye Workshop. The investigators quantified tear production by the Schirmer I test without anesthesia, assessed disease severity using the Ocular Surface Disease Index questionnaire and clinically evaluated the quality of the meibomian secretion, lid margin inflammation and corneal dye staining. All participants applied a warm compress to the eyes for 5 minutes daily. In this double-blind stu dy, participants were randomly assigned to consume 3 capsules daily, one per meal, of the n-3 LC-PUFAs plus antioxidants or a sunflower oil placebo without antioxidants. The total dose of n-3 LC-PUFAs per day was 1.3 g, providing 1.05 g of DHA, 128 mg of EPA and 30 mg DPA. Other capsule constituents included vitamins A, C, E, tyrosine, cysteine, glutathione, zinc, copper, manganese and selenium. Supplementation continued for 3 months, with objective assessments taken at monthly participant visits after baseline. Sixty-one participants completed the study.
dy, participants were randomly assigned to consume 3 capsules daily, one per meal, of the n-3 LC-PUFAs plus antioxidants or a sunflower oil placebo without antioxidants. The total dose of n-3 LC-PUFAs per day was 1.3 g, providing 1.05 g of DHA, 128 mg of EPA and 30 mg DPA. Other capsule constituents included vitamins A, C, E, tyrosine, cysteine, glutathione, zinc, copper, manganese and selenium. Supplementation continued for 3 months, with objective assessments taken at monthly participant visits after baseline. Sixty-one participants completed the study. 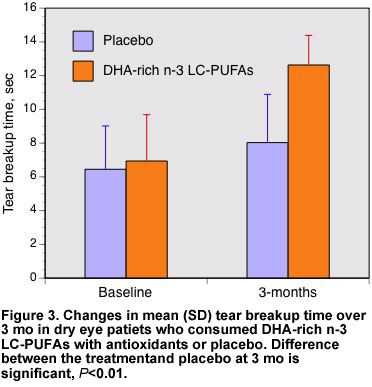 After 3 months, the tear breakup time was significantly increased in the n-3 LC-PUFA-supplemented participants with no significant change in the placebo group (Figure 3). Increased breakup time indicates a more stable tear film. Significant improvements compared with the control group were apparent at each monthly assessment. Cornea staining and tear quantity did not differ between the groups or from baseline values. Other significant improvements with n-3 LC-PUFA supplementation included decreased lid inflammation compared with baseline and increased meibomian gland expressibility. Both groups experienced significant decreases in the severity of their symptoms, such as sensitivity to light, soreness and a gritty feeling in the eyes. The study did not control for the antioxidants consumed with the n-3 LC-PUFA supplement, so the results cannot entirely be attributed to the effect of the n-3 PUFAs. However, the results are consistent with other findings in dry eye studies attributable to n-3 LC-PUFAs. This study demonstrated that 3 months’ consumption of a moderately high dose of DHA-rich n-3 LC-PUFAs was associated with a significant improvement in tear stability, reduction in eyelid inflammation and decreased clinical symptoms of meibomian gland dysfunction. These findings are consistent with the increased tear production observed in mice with dry eye treated with resolvin E1, a derivative of EPA; with clinical improvements in patients with keratoconjunctivitis sicca who consumed n-3 PUFAs and gamma-linolenic acid for 6 months; and with significant improvements in a short-term clinical study of patients with dry eye who consumed 600 mg/day of n-3 LC-PUFAs.
After 3 months, the tear breakup time was significantly increased in the n-3 LC-PUFA-supplemented participants with no significant change in the placebo group (Figure 3). Increased breakup time indicates a more stable tear film. Significant improvements compared with the control group were apparent at each monthly assessment. Cornea staining and tear quantity did not differ between the groups or from baseline values. Other significant improvements with n-3 LC-PUFA supplementation included decreased lid inflammation compared with baseline and increased meibomian gland expressibility. Both groups experienced significant decreases in the severity of their symptoms, such as sensitivity to light, soreness and a gritty feeling in the eyes. The study did not control for the antioxidants consumed with the n-3 LC-PUFA supplement, so the results cannot entirely be attributed to the effect of the n-3 PUFAs. However, the results are consistent with other findings in dry eye studies attributable to n-3 LC-PUFAs. This study demonstrated that 3 months’ consumption of a moderately high dose of DHA-rich n-3 LC-PUFAs was associated with a significant improvement in tear stability, reduction in eyelid inflammation and decreased clinical symptoms of meibomian gland dysfunction. These findings are consistent with the increased tear production observed in mice with dry eye treated with resolvin E1, a derivative of EPA; with clinical improvements in patients with keratoconjunctivitis sicca who consumed n-3 PUFAs and gamma-linolenic acid for 6 months; and with significant improvements in a short-term clinical study of patients with dry eye who consumed 600 mg/day of n-3 LC-PUFAs.  One can speculate that the anti-inflammatory effects of n-3 LC-PUFAs contributed to the observed clinical improvements, but other than reduced eyelid inflammation and clinical symptoms, no objective measures of inflammatory markers were performed. However, the anti-inflammatory effects of this supplement were described in a similar study using a lower dose of the same preparation. The investigators reported significantly improved clinical symptoms and significantly lower tear levels of IL-1β, ΙL-6 and IL-10 after 3 months’ supplementation with the DHA-rich n-3 LC-PUFAs and antioxidants. The present study provides a clear demonstration that DHA-rich n-3 LC-PUFA supplementation improves clinical and objective measures of meibomian gland dysfunction as observed in patients with dry eye syndrome. Even though the literature is not extensive, it has become common for optometrists, clinics and patient education materials to suggest increased consumption of omega-3 PUFAs for patients with dry eye disease. More good reasons to do so are emerging. Oleñik A, Jiménez-Alfaro I, Alejandre-Alba N, Mahillo-Fernández I. A randomized, double-masked study to evaluate the effect of omega-3 fatty acids supplementation in meibomian gland dysfunction. Clin Interv Aging 2013;8:1133-1138. [PubMed] Open Access Worth Noting Sheppard JD Jr, Singh R, McClellan AJ, Weikert MP, Scoper SV, Joly TJ, Whitley WO, Kakkar E, Pflugfelder SC. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: A randomized double-blind clinical trial. Cornea 2013; Jul 23. [Epub ahead of print] [PubMed] Kangari H, Eftekhari MH, Sardari S, Hashemi H, Salamzadeh J, Ghassemi-Broumand M, Khabazkhoob M. Short-term consumption of oral omega-3 and dry eye syndrome. Ophthalmology 2013;120:2191-2196. [PubMed] Kenchegowda S, He J, Bazan HE. Involvement of pigment epithelium-derived factor, docosahexaenoic acid and neuroprotectin D1 in corneal inflammation and nerve integrity after refractive surgery. Prostaglandins Leukot Essent Fatty Acids 2013;88:27-31. [PubMed] Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One 2013;8:e76121. [PubMed] Open Access
One can speculate that the anti-inflammatory effects of n-3 LC-PUFAs contributed to the observed clinical improvements, but other than reduced eyelid inflammation and clinical symptoms, no objective measures of inflammatory markers were performed. However, the anti-inflammatory effects of this supplement were described in a similar study using a lower dose of the same preparation. The investigators reported significantly improved clinical symptoms and significantly lower tear levels of IL-1β, ΙL-6 and IL-10 after 3 months’ supplementation with the DHA-rich n-3 LC-PUFAs and antioxidants. The present study provides a clear demonstration that DHA-rich n-3 LC-PUFA supplementation improves clinical and objective measures of meibomian gland dysfunction as observed in patients with dry eye syndrome. Even though the literature is not extensive, it has become common for optometrists, clinics and patient education materials to suggest increased consumption of omega-3 PUFAs for patients with dry eye disease. More good reasons to do so are emerging. Oleñik A, Jiménez-Alfaro I, Alejandre-Alba N, Mahillo-Fernández I. A randomized, double-masked study to evaluate the effect of omega-3 fatty acids supplementation in meibomian gland dysfunction. Clin Interv Aging 2013;8:1133-1138. [PubMed] Open Access Worth Noting Sheppard JD Jr, Singh R, McClellan AJ, Weikert MP, Scoper SV, Joly TJ, Whitley WO, Kakkar E, Pflugfelder SC. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: A randomized double-blind clinical trial. Cornea 2013; Jul 23. [Epub ahead of print] [PubMed] Kangari H, Eftekhari MH, Sardari S, Hashemi H, Salamzadeh J, Ghassemi-Broumand M, Khabazkhoob M. Short-term consumption of oral omega-3 and dry eye syndrome. Ophthalmology 2013;120:2191-2196. [PubMed] Kenchegowda S, He J, Bazan HE. Involvement of pigment epithelium-derived factor, docosahexaenoic acid and neuroprotectin D1 in corneal inflammation and nerve integrity after refractive surgery. Prostaglandins Leukot Essent Fatty Acids 2013;88:27-31. [PubMed] Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One 2013;8:e76121. [PubMed] Open Access

