Cardio-Protective Effects of Omega-3 LCPUFA in Percutaneous Coronary Intervention Reperfusion Therapy after ST-Segment Elevation Acute Myocardial Infarction
This article at a glance  disruption, or dissolution of a blood clot obstructing a coronary artery by percutaneous coronary intervention (PCI) or thrombolysis is live-saving. It limits the size of an infarct, preserves contractile function of the left ventricle, and reduces the development of heart failure. However, PCI and thrombolytic therapy also impart their own risks, which are related to so-called ischemia/reperfusion (I/R) tissue injury. The reperfusion of a temporally-occluded part of any organ can contribute to a significant extent to loss of viable organ tissue. Activation of oxygen- and nitrogen radical-mediated tissue damage occurs upon reoxygenation, as well as aberrant activation of neutrophil-dominated inflammation. In PCI, a widely employed surgical procedure to re-open one or more blocked coronary arteries, reperfusion of the affected ischemic tissue will occur, causing a certain degree of ischemia-reperfusion injury depending on the time of ischemia until PCI or thrombolysis, and on the endogenous tissue-protective and anti-inflammatory local mechanisms that are operative. The success of reperfusion therapy is an important determinant for clinical outcome. Pharmacological and mechanical approaches to protect myocardial tissue from reperfusion injury have been developed. Progress in PCI techniques and improved thrombolytic approaches, as well as an improved mechanistic understanding of myocardial I/R injury, and of secondary microvascular obstruction, and microvascular damage with intramyocardial hemorrhage, after PCI, will likely bring about further improvements. Still, even with much understanding and many intervention and treatment options, ischemic heart disease remains the most common cause of death in many countries in the world.
disruption, or dissolution of a blood clot obstructing a coronary artery by percutaneous coronary intervention (PCI) or thrombolysis is live-saving. It limits the size of an infarct, preserves contractile function of the left ventricle, and reduces the development of heart failure. However, PCI and thrombolytic therapy also impart their own risks, which are related to so-called ischemia/reperfusion (I/R) tissue injury. The reperfusion of a temporally-occluded part of any organ can contribute to a significant extent to loss of viable organ tissue. Activation of oxygen- and nitrogen radical-mediated tissue damage occurs upon reoxygenation, as well as aberrant activation of neutrophil-dominated inflammation. In PCI, a widely employed surgical procedure to re-open one or more blocked coronary arteries, reperfusion of the affected ischemic tissue will occur, causing a certain degree of ischemia-reperfusion injury depending on the time of ischemia until PCI or thrombolysis, and on the endogenous tissue-protective and anti-inflammatory local mechanisms that are operative. The success of reperfusion therapy is an important determinant for clinical outcome. Pharmacological and mechanical approaches to protect myocardial tissue from reperfusion injury have been developed. Progress in PCI techniques and improved thrombolytic approaches, as well as an improved mechanistic understanding of myocardial I/R injury, and of secondary microvascular obstruction, and microvascular damage with intramyocardial hemorrhage, after PCI, will likely bring about further improvements. Still, even with much understanding and many intervention and treatment options, ischemic heart disease remains the most common cause of death in many countries in the world. 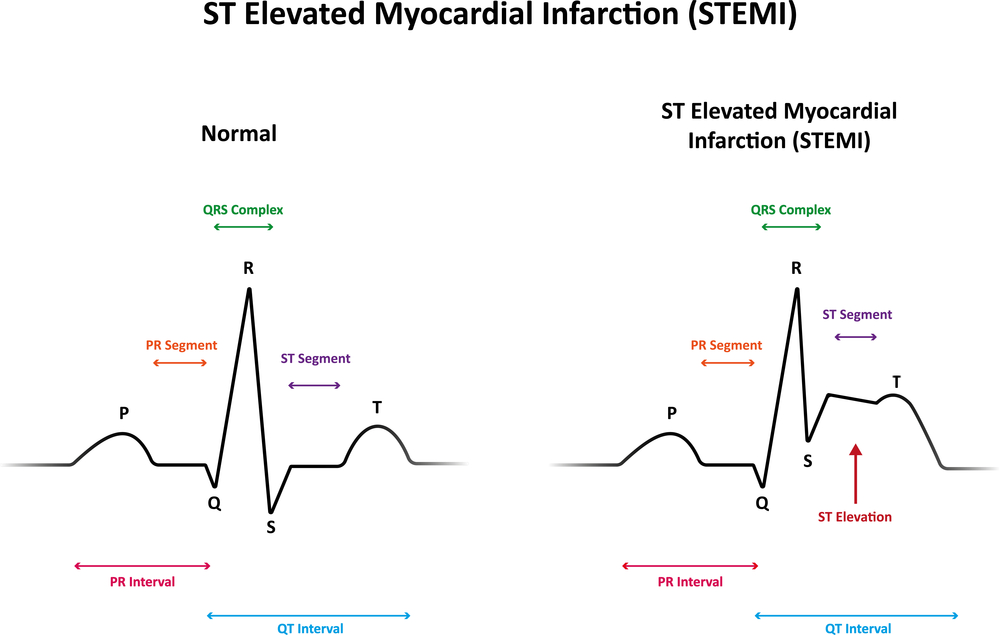 Narrowing Down Patient Variables A role for omega-3 LCPUFA in protecting the myocardium has not been formally demonstrated within the context of reperfusion therapy in ischemic heart disease in humans. DHA is known to be rapidly incorporated and retained in myocardial membrane lipids, and may play a regulatory function in myocardial electrophysiology. A recent observational study has addressed the potential association of serum omega-3 LCPUFA levels with I/R-injury and clinical effects of myocardial damage in patients with ST-segment elevation acute myocardial infarction (STEMI) that underwent PCI. The research was by Dr. Kantaro Arakawa at the Division of Cardiology at Fujisawa Hospital in Kanagawa, Japan, together with colleagues from Yokohama City University Hospital Medical Center and School of Medicine. Data from 221 patients with STEMI were analyzed to identify which patient variables correlated with ST-segment re-elevation and reperfusion arrhythmias as outcome of myocardial reperfusion injury.
Narrowing Down Patient Variables A role for omega-3 LCPUFA in protecting the myocardium has not been formally demonstrated within the context of reperfusion therapy in ischemic heart disease in humans. DHA is known to be rapidly incorporated and retained in myocardial membrane lipids, and may play a regulatory function in myocardial electrophysiology. A recent observational study has addressed the potential association of serum omega-3 LCPUFA levels with I/R-injury and clinical effects of myocardial damage in patients with ST-segment elevation acute myocardial infarction (STEMI) that underwent PCI. The research was by Dr. Kantaro Arakawa at the Division of Cardiology at Fujisawa Hospital in Kanagawa, Japan, together with colleagues from Yokohama City University Hospital Medical Center and School of Medicine. Data from 221 patients with STEMI were analyzed to identify which patient variables correlated with ST-segment re-elevation and reperfusion arrhythmias as outcome of myocardial reperfusion injury.  These patients had shown ST–segment re-elevation on electrocardiograms recorded during pre-hospital cardiopulmonary resuscitation, stenosis of ≥90% of lesion diameter, a TIMI flow grade of 0 or 1 (a standardized measure of coronary blood flow), and an increase in serum creatinine kinase that surpassed twice the maximal normal level. Emergency PCI had been performed within six hours after chest pain onset. The patients included 160 men and 51 women, with an average age of 67 years. Blood samples were analyzed for fatty acid composition of serum after transmethylation of all serum lipids. Infarct size was estimated using the serial QRS scoring system prior to PCI, one hour after PCI, and at hospital discharge. In order to appreciate if the blood levels of omega-3 LCPUFA might carry any predictive value to the extent of myocardial I/R injury, the patients were divided into two equally sized groups on the basis of the sum of EPA and DHA before angiography (median 155.0 microgram/ml), one (group L) had EPA ± DHA levels < 155 microgram/ml (n=106), and the second group (H) had levels ≥ 155 microgram/ml (n=105). Besides the significantly different blood levels of EPA and DHA, the baseline clinical characteristics of these two groups did not show significant differences for a range of variables related to other disease incidence, drug use, clinical chemistry, blood pressure and heart rate, and an estimation of the myocardial area at risk. Some differences were noted: a lower percentage of smokers in group H (29% vs 52%), and a higher use of calcium channel blockers in group H (33% vs 19%). Group H also showed a small but significant increase in the level of arachidonic acid, but the ratio of EPA to AA was more than two-fold higher in group H compared to group L. Results
These patients had shown ST–segment re-elevation on electrocardiograms recorded during pre-hospital cardiopulmonary resuscitation, stenosis of ≥90% of lesion diameter, a TIMI flow grade of 0 or 1 (a standardized measure of coronary blood flow), and an increase in serum creatinine kinase that surpassed twice the maximal normal level. Emergency PCI had been performed within six hours after chest pain onset. The patients included 160 men and 51 women, with an average age of 67 years. Blood samples were analyzed for fatty acid composition of serum after transmethylation of all serum lipids. Infarct size was estimated using the serial QRS scoring system prior to PCI, one hour after PCI, and at hospital discharge. In order to appreciate if the blood levels of omega-3 LCPUFA might carry any predictive value to the extent of myocardial I/R injury, the patients were divided into two equally sized groups on the basis of the sum of EPA and DHA before angiography (median 155.0 microgram/ml), one (group L) had EPA ± DHA levels < 155 microgram/ml (n=106), and the second group (H) had levels ≥ 155 microgram/ml (n=105). Besides the significantly different blood levels of EPA and DHA, the baseline clinical characteristics of these two groups did not show significant differences for a range of variables related to other disease incidence, drug use, clinical chemistry, blood pressure and heart rate, and an estimation of the myocardial area at risk. Some differences were noted: a lower percentage of smokers in group H (29% vs 52%), and a higher use of calcium channel blockers in group H (33% vs 19%). Group H also showed a small but significant increase in the level of arachidonic acid, but the ratio of EPA to AA was more than two-fold higher in group H compared to group L. Results  The researchers did not find any correlation between the time of blood sampling after symptom onset and EPA+DHA levels in blood, indicating that acute myocardial infraction did not alter blood omega-3 LCPUFA levels. In patients of group L the increase in QRS score after PCI was significantly higher than in group H, indicating that infarct size was considerably higher (Table 1). It remained high upon hospital discharge, suggesting that myocardial scarring remained significantly greater in patients with a lower blood omega-3 LCPUFA levels. Immediately after PCI-initiated reperfusion, both ST-segment re-elevation and reperfusion ventricular arrhythmias were significantly lower in group H patients (Table 1). These findings indicate that I/R injury is substantially reduced in patients with higher EPA+DHA levels. Serum EPA+DHA levels correlated well with I/R injury when analyzed by univariate and multivariate regression analysis. Having pre-myocardial infarction angina, as well as the length of ischemia prior to PCI, also correlated significantly with I/R injury. Based on the results, the authors calculated a highest predictive level (a combination of optimal sensitivity (true positive rate) and specificity (true negative rate)) of serum EPA+DHA level in calculating ST-segment re-elevation of 157 microgram/ml. For reperfusion arrhythmias, 135 microgram/ml had the highest predictive value.
The researchers did not find any correlation between the time of blood sampling after symptom onset and EPA+DHA levels in blood, indicating that acute myocardial infraction did not alter blood omega-3 LCPUFA levels. In patients of group L the increase in QRS score after PCI was significantly higher than in group H, indicating that infarct size was considerably higher (Table 1). It remained high upon hospital discharge, suggesting that myocardial scarring remained significantly greater in patients with a lower blood omega-3 LCPUFA levels. Immediately after PCI-initiated reperfusion, both ST-segment re-elevation and reperfusion ventricular arrhythmias were significantly lower in group H patients (Table 1). These findings indicate that I/R injury is substantially reduced in patients with higher EPA+DHA levels. Serum EPA+DHA levels correlated well with I/R injury when analyzed by univariate and multivariate regression analysis. Having pre-myocardial infarction angina, as well as the length of ischemia prior to PCI, also correlated significantly with I/R injury. Based on the results, the authors calculated a highest predictive level (a combination of optimal sensitivity (true positive rate) and specificity (true negative rate)) of serum EPA+DHA level in calculating ST-segment re-elevation of 157 microgram/ml. For reperfusion arrhythmias, 135 microgram/ml had the highest predictive value. 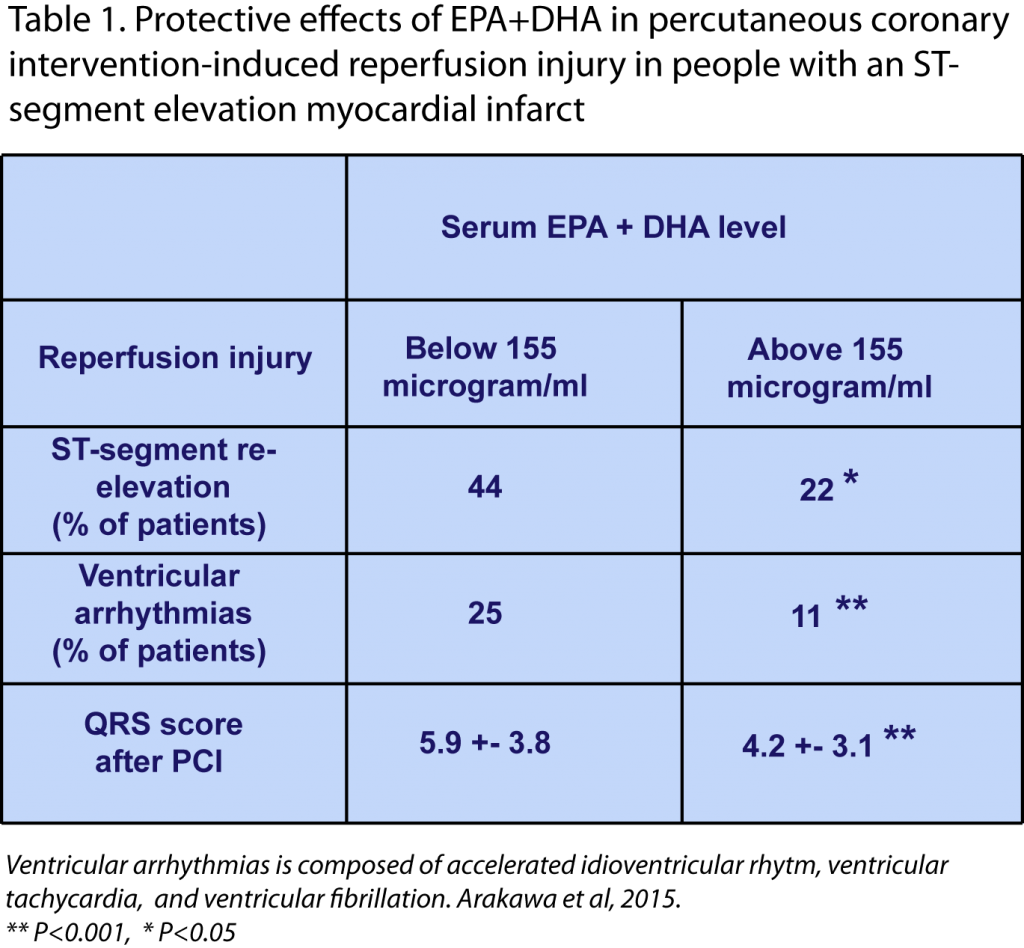 In summary, this study provides interesting new indications that in people with an acute myocardial infarction (STEMI type) and that are treated with PCI reperfusion therapy within six hours of symptoms onset, lower levels of EPA+DHA associate with a significantly increased risk of I/R injury, namely ST-segment re-elevation, reperfusion arrhythmia, and the extent of myocardial damage. The authors discuss that acute administration of omega-3 LCPUFA before or after PCI might be an adjunctive therapy to offer cardioprotection against I/R injury. This approach could be more effective in patients with a first AMI. This view is based on the fact that other studies in patients with a recurrent ventricular fibrillation have not consistently shown a measurable benefit from omega-3 LCPUFA supplementation, which the authors ascribe to concomitant therapies. The limitation of the current study is that it is an observational study, and other parameters were associated with blood levels of omega-3 LCPUFA (smoking, calcium blockers), or with a change in reperfusion injury incidence (presence of existing angina, length of ischemia). The study is of significant interest since a logical link can be postulated between the known actions of omega-3 LCPUFA and the observed protection. Confirmation of this proposed role awaits a controlled intervention trial in patients with angina that are at risk for STEMI and undergoing PCI as a preferred reperfusion treatment. Protective Actions during Myocardial Infarction The authors indicate that the mechanisms whereby omega-3 LCPUFA may reduce myocardial reperfusion injury remain to be established. A recently published study led by Ganesh Halade and colleagues at the Division of Cardiovascular Disease, Department of Medicine at the University of Alabama, Birmingham, AL, USA, has addressed how such an omega-3 LPUFA-mediated protective action may be mediated. Together with colleagues at the Center for Experimental Therapeutics and Reperfusion Injury at Brigham & Women’s Hospital, Boston, MA and the Chicago College of Pharmacy at Midwestern University, IL, the investigators examined the molecular and cellular events during ischemia-induced inflammatory damage following myocardial infarction. In a murine model of myocardial ischemia-induced infarction by permanent ligation of the left descending coronary artery, left ventricular dysfunction was induced after one to five days, as a model for ventricular remodeling and heart failure. Functional read-outs for left ventricular function were the fractional shortening (ratio between the diameter of the left ventricle when relaxed and the diameter when it is contracted), end-diastolic dimension (diameter across the left ventricle at the end of diastole), end-systolic dimension, infarcted wall thickness, and heart rate. The research addressed if the DHA-derived lipid mediator resolvin D1 (RvD1) affected ischemic ventricular remodeling and function. Results After one and five days, fractional shortening of the ventricle was markedly reduced, and ventricle diameter at systole and diastole significantly increased. The thickness of the infarcted myocardial lesion was markedly reduced. The sub-cutaneous administration of small doses of RvD1 (3 microgram/kg/day), either as the free acid or incorporated within multi-lamellar liposomes, significantly reduced the remodeling of the ventricle. RvD1 increased neutrophilic infiltration at day 1, but ablated the presence of neutrophils in the ventricle at day 5. RvD1 upregulated the expression of 5-lipoxygenase (a biosynthetic enzyme involved in wound healing and synthesis of lipid mediators), the receptor for RvD1 and lipoxin A4, an arachidonic acid-derived lipid mediator with anti-inflammatory activity. A small decrease in the number of macrophages was also induced by RvD1, and importantly the phenotype of myocardial macrophages changed from a predominant M1 classical macrophage phenotype to an M2 macrophage phenotype that play a role in resolving inflammation. Collagen deposition in the ventricle at day 5 was significantly reduced by RvD1. The functional effects of myocardial ischemia were not limited to a local response. A marked edema of the lungs appeared after one day, which was abrogated by RvD1. Following myocardial ischemia the spleen reacted rapidly with a marked reduction in weight. The involvement of the spleen, with the mobilization of pro-inflammatory leukocytes, has recently been recognized to be activated after acute myocardial infarct in humans. Also in the spleen macrophages expressed predominantly the M2 macrophage phenotype. Discussion These studies provide new insight into the potentially protective roles of omega-3 LCPUFA in the myocardium after an AMI. The studies are important since a better understanding of their role in protection from ischemia, ischemia-reperfusion injury, and incomplete reperfusion therapy, will likely help in refining interventions after acute myocardial insults. The mouse study did not address the involvement of a DHA-derived lipid mediator in reperfusion injury, but rather in a setting of prolonged ischemia-induced ventricular injury. It highlights the possibly important role of splenic activation following a myocardial infarct, and the omega-3 LCPUFA-derived lipid mediators that are formed there may play a role in activating splenic retention of immune cells that mediate ventricular damage. Further studies that directly address the relationship between blood levels or dietary intake of omega-3 LCPUFA and outcome of myocardial I/R injury and reperfusion approaches are now of significant interest and clinical value. Arakawa K, Himeno H, Kirigaya J, Otomo F, Matsushita K, Nakahashi H, Shimizu S, Nitta M, Yano H, Endo M, Kimura K, Umemura S. Impact of n-3 polyunsaturated fatty acids in predicting ischemia/reperfusion injury and progression of myocardial damage after reperfusion in patients with ST-segment elevation acute myocardial infarction. J. Cardiol. 2015;Apr. 3. [PubMed] Kain V, Ingle KA, Colas RA, Dalli J, Prabhu SD, Serhan CN, Joshi M, Halade GV. Resolvin D1 activates the inflammation resolving response at splenic and ventricular site following myocardial infarction leading to improved ventricular function. J. Mol. Cell. Cardiol. 2015;84:24-35. [PubMed] Worth Noting Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation 2013;127(24):2452-2457. [PubMed] Claeys MJ, Bosmans J, De Ceuninck M, Beunis A, Vergauwen W, Vorlat A, Vrints CJ. Effect of intracoronary adenosine infusion during coronary intervention on myocardial reperfusion injury in patients with acute myocardial infarction. Am. J. Cardiol. 2004;94(1):9-13. [PubMed] Emami H, Singh P, MacNabb M, Vucic E, Lavender Z, Rudd JH, Fayad ZA, Lehrer-Graiwer J, Korsgren M, Figueroa AL, Fredrickson J, Rubin B, Hoffmann U, Truong QA, Min JK, Baruch A, Nasir K, Nahrendorf M, Tawakol A. Splenic metabolic activity predicts risk of future cardiovascular events: demonstration of a cardiosplenic axis in humans. J.A.C.C. Cardiovasc. Imaging 2015;8(2):121-130. [PubMed] Fröhlich GM, Meier P, White SK, Yellon DM, Hausenloy DJ. Myocardial reperfusion injury: looking beyond primary PCI. Eur. Heart J. 2013;34(23):1714-1722. [PubMed] Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van De Werf F, Braunwald E. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101(2):125-130. [PubMed] James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br. J. Nutr. 2014;112(5):812-820. [PubMed] Kapela A, Bezerianos A. A theoretical model of the high-frequency arrhythmogenic depolarization signal following myocardial infarction. IEEE Trans. Biomed. Eng. 2004;51(11):1915-1922. [PubMed] van Lavieren MA, van de Hoef TP, Piek JJ. Primary PCI: time to change focus from epicardial reperfusion towards protection of the microvasculature. EuroIntervention 2014;10 (Suppl T):T39-46. [PubMed] Loring Z, Chelliah S, Selvester RH, Wagner G, Strauss DG. A detailed guide for quantification of myocardial scar with the Selvester QRS score in the presence of electrocardiogram confounders. J. Electrocardiol. 2011;44(5):544-554. [PubMed] McLennan PL. Myocardial membrane fatty acids and the antiarrhythmic actions of dietary fish oil in animal models. Lipids 2001;36 Suppl.:S111-114. [PubMed] Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD, Cleland LG. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am. J. Clin. Nutr. 2007;85(5):1222-1228. [PubMed] Mori TA. Omega-3 fatty acids and cardiovascular disease: epidemiology and effects on cardiometabolic risk factors. Food Funct. 2014;5(9):2004-2019. [PubMed] Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 Global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014;174(2):293-298. [PubMed] von Schacky C. Cardiovascular disease prevention and treatment. Prostaglandins Leukot. Essent. Fatty Acids 2009;81(2-3):193-198. [PubMed] Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U, European Association for Percutaneous Cardiovascular I. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur. Heart J. 2010;31(8):943-957. [PubMed] TIMI : TIMI Study Group http://www.timi.org/ Visual Sonics – In vivo imaging system : http://www.visualsonics.com/
In summary, this study provides interesting new indications that in people with an acute myocardial infarction (STEMI type) and that are treated with PCI reperfusion therapy within six hours of symptoms onset, lower levels of EPA+DHA associate with a significantly increased risk of I/R injury, namely ST-segment re-elevation, reperfusion arrhythmia, and the extent of myocardial damage. The authors discuss that acute administration of omega-3 LCPUFA before or after PCI might be an adjunctive therapy to offer cardioprotection against I/R injury. This approach could be more effective in patients with a first AMI. This view is based on the fact that other studies in patients with a recurrent ventricular fibrillation have not consistently shown a measurable benefit from omega-3 LCPUFA supplementation, which the authors ascribe to concomitant therapies. The limitation of the current study is that it is an observational study, and other parameters were associated with blood levels of omega-3 LCPUFA (smoking, calcium blockers), or with a change in reperfusion injury incidence (presence of existing angina, length of ischemia). The study is of significant interest since a logical link can be postulated between the known actions of omega-3 LCPUFA and the observed protection. Confirmation of this proposed role awaits a controlled intervention trial in patients with angina that are at risk for STEMI and undergoing PCI as a preferred reperfusion treatment. Protective Actions during Myocardial Infarction The authors indicate that the mechanisms whereby omega-3 LCPUFA may reduce myocardial reperfusion injury remain to be established. A recently published study led by Ganesh Halade and colleagues at the Division of Cardiovascular Disease, Department of Medicine at the University of Alabama, Birmingham, AL, USA, has addressed how such an omega-3 LPUFA-mediated protective action may be mediated. Together with colleagues at the Center for Experimental Therapeutics and Reperfusion Injury at Brigham & Women’s Hospital, Boston, MA and the Chicago College of Pharmacy at Midwestern University, IL, the investigators examined the molecular and cellular events during ischemia-induced inflammatory damage following myocardial infarction. In a murine model of myocardial ischemia-induced infarction by permanent ligation of the left descending coronary artery, left ventricular dysfunction was induced after one to five days, as a model for ventricular remodeling and heart failure. Functional read-outs for left ventricular function were the fractional shortening (ratio between the diameter of the left ventricle when relaxed and the diameter when it is contracted), end-diastolic dimension (diameter across the left ventricle at the end of diastole), end-systolic dimension, infarcted wall thickness, and heart rate. The research addressed if the DHA-derived lipid mediator resolvin D1 (RvD1) affected ischemic ventricular remodeling and function. Results After one and five days, fractional shortening of the ventricle was markedly reduced, and ventricle diameter at systole and diastole significantly increased. The thickness of the infarcted myocardial lesion was markedly reduced. The sub-cutaneous administration of small doses of RvD1 (3 microgram/kg/day), either as the free acid or incorporated within multi-lamellar liposomes, significantly reduced the remodeling of the ventricle. RvD1 increased neutrophilic infiltration at day 1, but ablated the presence of neutrophils in the ventricle at day 5. RvD1 upregulated the expression of 5-lipoxygenase (a biosynthetic enzyme involved in wound healing and synthesis of lipid mediators), the receptor for RvD1 and lipoxin A4, an arachidonic acid-derived lipid mediator with anti-inflammatory activity. A small decrease in the number of macrophages was also induced by RvD1, and importantly the phenotype of myocardial macrophages changed from a predominant M1 classical macrophage phenotype to an M2 macrophage phenotype that play a role in resolving inflammation. Collagen deposition in the ventricle at day 5 was significantly reduced by RvD1. The functional effects of myocardial ischemia were not limited to a local response. A marked edema of the lungs appeared after one day, which was abrogated by RvD1. Following myocardial ischemia the spleen reacted rapidly with a marked reduction in weight. The involvement of the spleen, with the mobilization of pro-inflammatory leukocytes, has recently been recognized to be activated after acute myocardial infarct in humans. Also in the spleen macrophages expressed predominantly the M2 macrophage phenotype. Discussion These studies provide new insight into the potentially protective roles of omega-3 LCPUFA in the myocardium after an AMI. The studies are important since a better understanding of their role in protection from ischemia, ischemia-reperfusion injury, and incomplete reperfusion therapy, will likely help in refining interventions after acute myocardial insults. The mouse study did not address the involvement of a DHA-derived lipid mediator in reperfusion injury, but rather in a setting of prolonged ischemia-induced ventricular injury. It highlights the possibly important role of splenic activation following a myocardial infarct, and the omega-3 LCPUFA-derived lipid mediators that are formed there may play a role in activating splenic retention of immune cells that mediate ventricular damage. Further studies that directly address the relationship between blood levels or dietary intake of omega-3 LCPUFA and outcome of myocardial I/R injury and reperfusion approaches are now of significant interest and clinical value. Arakawa K, Himeno H, Kirigaya J, Otomo F, Matsushita K, Nakahashi H, Shimizu S, Nitta M, Yano H, Endo M, Kimura K, Umemura S. Impact of n-3 polyunsaturated fatty acids in predicting ischemia/reperfusion injury and progression of myocardial damage after reperfusion in patients with ST-segment elevation acute myocardial infarction. J. Cardiol. 2015;Apr. 3. [PubMed] Kain V, Ingle KA, Colas RA, Dalli J, Prabhu SD, Serhan CN, Joshi M, Halade GV. Resolvin D1 activates the inflammation resolving response at splenic and ventricular site following myocardial infarction leading to improved ventricular function. J. Mol. Cell. Cardiol. 2015;84:24-35. [PubMed] Worth Noting Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation 2013;127(24):2452-2457. [PubMed] Claeys MJ, Bosmans J, De Ceuninck M, Beunis A, Vergauwen W, Vorlat A, Vrints CJ. Effect of intracoronary adenosine infusion during coronary intervention on myocardial reperfusion injury in patients with acute myocardial infarction. Am. J. Cardiol. 2004;94(1):9-13. [PubMed] Emami H, Singh P, MacNabb M, Vucic E, Lavender Z, Rudd JH, Fayad ZA, Lehrer-Graiwer J, Korsgren M, Figueroa AL, Fredrickson J, Rubin B, Hoffmann U, Truong QA, Min JK, Baruch A, Nasir K, Nahrendorf M, Tawakol A. Splenic metabolic activity predicts risk of future cardiovascular events: demonstration of a cardiosplenic axis in humans. J.A.C.C. Cardiovasc. Imaging 2015;8(2):121-130. [PubMed] Fröhlich GM, Meier P, White SK, Yellon DM, Hausenloy DJ. Myocardial reperfusion injury: looking beyond primary PCI. Eur. Heart J. 2013;34(23):1714-1722. [PubMed] Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van De Werf F, Braunwald E. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101(2):125-130. [PubMed] James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br. J. Nutr. 2014;112(5):812-820. [PubMed] Kapela A, Bezerianos A. A theoretical model of the high-frequency arrhythmogenic depolarization signal following myocardial infarction. IEEE Trans. Biomed. Eng. 2004;51(11):1915-1922. [PubMed] van Lavieren MA, van de Hoef TP, Piek JJ. Primary PCI: time to change focus from epicardial reperfusion towards protection of the microvasculature. EuroIntervention 2014;10 (Suppl T):T39-46. [PubMed] Loring Z, Chelliah S, Selvester RH, Wagner G, Strauss DG. A detailed guide for quantification of myocardial scar with the Selvester QRS score in the presence of electrocardiogram confounders. J. Electrocardiol. 2011;44(5):544-554. [PubMed] McLennan PL. Myocardial membrane fatty acids and the antiarrhythmic actions of dietary fish oil in animal models. Lipids 2001;36 Suppl.:S111-114. [PubMed] Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD, Cleland LG. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am. J. Clin. Nutr. 2007;85(5):1222-1228. [PubMed] Mori TA. Omega-3 fatty acids and cardiovascular disease: epidemiology and effects on cardiometabolic risk factors. Food Funct. 2014;5(9):2004-2019. [PubMed] Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 Global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014;174(2):293-298. [PubMed] von Schacky C. Cardiovascular disease prevention and treatment. Prostaglandins Leukot. Essent. Fatty Acids 2009;81(2-3):193-198. [PubMed] Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U, European Association for Percutaneous Cardiovascular I. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur. Heart J. 2010;31(8):943-957. [PubMed] TIMI : TIMI Study Group http://www.timi.org/ Visual Sonics – In vivo imaging system : http://www.visualsonics.com/
- Acute myocardial infarction (AMI) remains one of the most common causes of death globally.
- The study reports the results of an observational study of Japanese patients who had a STEMI-type AMI and that received percutaneous coronary intervention (PCI) reperfusion therapy.
- The results indicate that people who had EPA + DHA levels in serum over 155 mg/ml had a markedly better outcome of PCI than people with low omega-3 LCPUFA levels; ischemia-reperfusion injury was decreased as measured by fewer reperfusion ventricular arrhythmias, lower ST-segment re-elevation, and less myocardial tissue injury.
 disruption, or dissolution of a blood clot obstructing a coronary artery by percutaneous coronary intervention (PCI) or thrombolysis is live-saving. It limits the size of an infarct, preserves contractile function of the left ventricle, and reduces the development of heart failure. However, PCI and thrombolytic therapy also impart their own risks, which are related to so-called ischemia/reperfusion (I/R) tissue injury. The reperfusion of a temporally-occluded part of any organ can contribute to a significant extent to loss of viable organ tissue. Activation of oxygen- and nitrogen radical-mediated tissue damage occurs upon reoxygenation, as well as aberrant activation of neutrophil-dominated inflammation. In PCI, a widely employed surgical procedure to re-open one or more blocked coronary arteries, reperfusion of the affected ischemic tissue will occur, causing a certain degree of ischemia-reperfusion injury depending on the time of ischemia until PCI or thrombolysis, and on the endogenous tissue-protective and anti-inflammatory local mechanisms that are operative. The success of reperfusion therapy is an important determinant for clinical outcome. Pharmacological and mechanical approaches to protect myocardial tissue from reperfusion injury have been developed. Progress in PCI techniques and improved thrombolytic approaches, as well as an improved mechanistic understanding of myocardial I/R injury, and of secondary microvascular obstruction, and microvascular damage with intramyocardial hemorrhage, after PCI, will likely bring about further improvements. Still, even with much understanding and many intervention and treatment options, ischemic heart disease remains the most common cause of death in many countries in the world.
disruption, or dissolution of a blood clot obstructing a coronary artery by percutaneous coronary intervention (PCI) or thrombolysis is live-saving. It limits the size of an infarct, preserves contractile function of the left ventricle, and reduces the development of heart failure. However, PCI and thrombolytic therapy also impart their own risks, which are related to so-called ischemia/reperfusion (I/R) tissue injury. The reperfusion of a temporally-occluded part of any organ can contribute to a significant extent to loss of viable organ tissue. Activation of oxygen- and nitrogen radical-mediated tissue damage occurs upon reoxygenation, as well as aberrant activation of neutrophil-dominated inflammation. In PCI, a widely employed surgical procedure to re-open one or more blocked coronary arteries, reperfusion of the affected ischemic tissue will occur, causing a certain degree of ischemia-reperfusion injury depending on the time of ischemia until PCI or thrombolysis, and on the endogenous tissue-protective and anti-inflammatory local mechanisms that are operative. The success of reperfusion therapy is an important determinant for clinical outcome. Pharmacological and mechanical approaches to protect myocardial tissue from reperfusion injury have been developed. Progress in PCI techniques and improved thrombolytic approaches, as well as an improved mechanistic understanding of myocardial I/R injury, and of secondary microvascular obstruction, and microvascular damage with intramyocardial hemorrhage, after PCI, will likely bring about further improvements. Still, even with much understanding and many intervention and treatment options, ischemic heart disease remains the most common cause of death in many countries in the world. 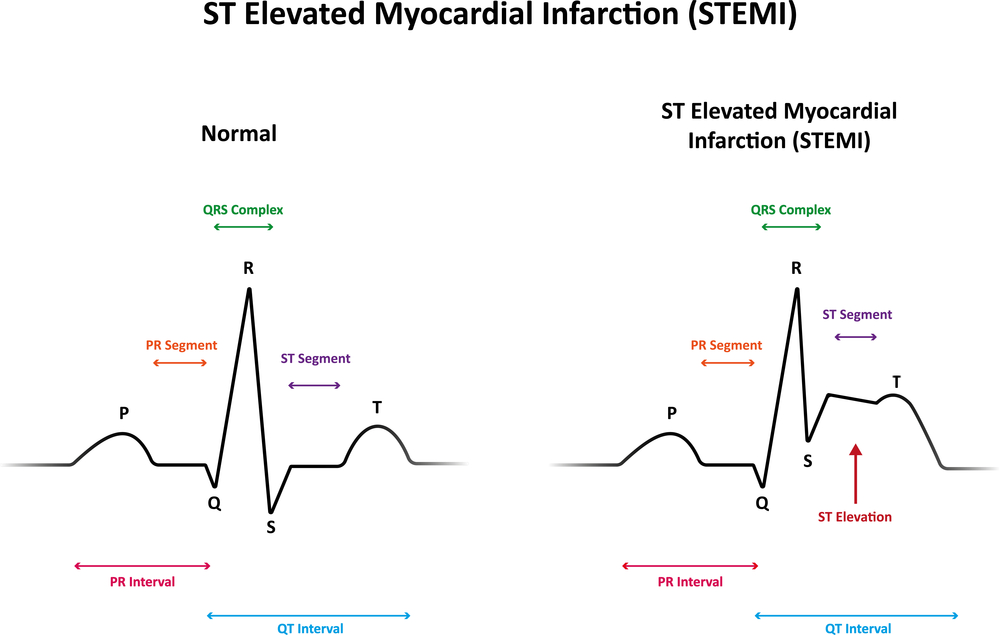 Narrowing Down Patient Variables A role for omega-3 LCPUFA in protecting the myocardium has not been formally demonstrated within the context of reperfusion therapy in ischemic heart disease in humans. DHA is known to be rapidly incorporated and retained in myocardial membrane lipids, and may play a regulatory function in myocardial electrophysiology. A recent observational study has addressed the potential association of serum omega-3 LCPUFA levels with I/R-injury and clinical effects of myocardial damage in patients with ST-segment elevation acute myocardial infarction (STEMI) that underwent PCI. The research was by Dr. Kantaro Arakawa at the Division of Cardiology at Fujisawa Hospital in Kanagawa, Japan, together with colleagues from Yokohama City University Hospital Medical Center and School of Medicine. Data from 221 patients with STEMI were analyzed to identify which patient variables correlated with ST-segment re-elevation and reperfusion arrhythmias as outcome of myocardial reperfusion injury.
Narrowing Down Patient Variables A role for omega-3 LCPUFA in protecting the myocardium has not been formally demonstrated within the context of reperfusion therapy in ischemic heart disease in humans. DHA is known to be rapidly incorporated and retained in myocardial membrane lipids, and may play a regulatory function in myocardial electrophysiology. A recent observational study has addressed the potential association of serum omega-3 LCPUFA levels with I/R-injury and clinical effects of myocardial damage in patients with ST-segment elevation acute myocardial infarction (STEMI) that underwent PCI. The research was by Dr. Kantaro Arakawa at the Division of Cardiology at Fujisawa Hospital in Kanagawa, Japan, together with colleagues from Yokohama City University Hospital Medical Center and School of Medicine. Data from 221 patients with STEMI were analyzed to identify which patient variables correlated with ST-segment re-elevation and reperfusion arrhythmias as outcome of myocardial reperfusion injury.  These patients had shown ST–segment re-elevation on electrocardiograms recorded during pre-hospital cardiopulmonary resuscitation, stenosis of ≥90% of lesion diameter, a TIMI flow grade of 0 or 1 (a standardized measure of coronary blood flow), and an increase in serum creatinine kinase that surpassed twice the maximal normal level. Emergency PCI had been performed within six hours after chest pain onset. The patients included 160 men and 51 women, with an average age of 67 years. Blood samples were analyzed for fatty acid composition of serum after transmethylation of all serum lipids. Infarct size was estimated using the serial QRS scoring system prior to PCI, one hour after PCI, and at hospital discharge. In order to appreciate if the blood levels of omega-3 LCPUFA might carry any predictive value to the extent of myocardial I/R injury, the patients were divided into two equally sized groups on the basis of the sum of EPA and DHA before angiography (median 155.0 microgram/ml), one (group L) had EPA ± DHA levels < 155 microgram/ml (n=106), and the second group (H) had levels ≥ 155 microgram/ml (n=105). Besides the significantly different blood levels of EPA and DHA, the baseline clinical characteristics of these two groups did not show significant differences for a range of variables related to other disease incidence, drug use, clinical chemistry, blood pressure and heart rate, and an estimation of the myocardial area at risk. Some differences were noted: a lower percentage of smokers in group H (29% vs 52%), and a higher use of calcium channel blockers in group H (33% vs 19%). Group H also showed a small but significant increase in the level of arachidonic acid, but the ratio of EPA to AA was more than two-fold higher in group H compared to group L. Results
These patients had shown ST–segment re-elevation on electrocardiograms recorded during pre-hospital cardiopulmonary resuscitation, stenosis of ≥90% of lesion diameter, a TIMI flow grade of 0 or 1 (a standardized measure of coronary blood flow), and an increase in serum creatinine kinase that surpassed twice the maximal normal level. Emergency PCI had been performed within six hours after chest pain onset. The patients included 160 men and 51 women, with an average age of 67 years. Blood samples were analyzed for fatty acid composition of serum after transmethylation of all serum lipids. Infarct size was estimated using the serial QRS scoring system prior to PCI, one hour after PCI, and at hospital discharge. In order to appreciate if the blood levels of omega-3 LCPUFA might carry any predictive value to the extent of myocardial I/R injury, the patients were divided into two equally sized groups on the basis of the sum of EPA and DHA before angiography (median 155.0 microgram/ml), one (group L) had EPA ± DHA levels < 155 microgram/ml (n=106), and the second group (H) had levels ≥ 155 microgram/ml (n=105). Besides the significantly different blood levels of EPA and DHA, the baseline clinical characteristics of these two groups did not show significant differences for a range of variables related to other disease incidence, drug use, clinical chemistry, blood pressure and heart rate, and an estimation of the myocardial area at risk. Some differences were noted: a lower percentage of smokers in group H (29% vs 52%), and a higher use of calcium channel blockers in group H (33% vs 19%). Group H also showed a small but significant increase in the level of arachidonic acid, but the ratio of EPA to AA was more than two-fold higher in group H compared to group L. Results  The researchers did not find any correlation between the time of blood sampling after symptom onset and EPA+DHA levels in blood, indicating that acute myocardial infraction did not alter blood omega-3 LCPUFA levels. In patients of group L the increase in QRS score after PCI was significantly higher than in group H, indicating that infarct size was considerably higher (Table 1). It remained high upon hospital discharge, suggesting that myocardial scarring remained significantly greater in patients with a lower blood omega-3 LCPUFA levels. Immediately after PCI-initiated reperfusion, both ST-segment re-elevation and reperfusion ventricular arrhythmias were significantly lower in group H patients (Table 1). These findings indicate that I/R injury is substantially reduced in patients with higher EPA+DHA levels. Serum EPA+DHA levels correlated well with I/R injury when analyzed by univariate and multivariate regression analysis. Having pre-myocardial infarction angina, as well as the length of ischemia prior to PCI, also correlated significantly with I/R injury. Based on the results, the authors calculated a highest predictive level (a combination of optimal sensitivity (true positive rate) and specificity (true negative rate)) of serum EPA+DHA level in calculating ST-segment re-elevation of 157 microgram/ml. For reperfusion arrhythmias, 135 microgram/ml had the highest predictive value.
The researchers did not find any correlation between the time of blood sampling after symptom onset and EPA+DHA levels in blood, indicating that acute myocardial infraction did not alter blood omega-3 LCPUFA levels. In patients of group L the increase in QRS score after PCI was significantly higher than in group H, indicating that infarct size was considerably higher (Table 1). It remained high upon hospital discharge, suggesting that myocardial scarring remained significantly greater in patients with a lower blood omega-3 LCPUFA levels. Immediately after PCI-initiated reperfusion, both ST-segment re-elevation and reperfusion ventricular arrhythmias were significantly lower in group H patients (Table 1). These findings indicate that I/R injury is substantially reduced in patients with higher EPA+DHA levels. Serum EPA+DHA levels correlated well with I/R injury when analyzed by univariate and multivariate regression analysis. Having pre-myocardial infarction angina, as well as the length of ischemia prior to PCI, also correlated significantly with I/R injury. Based on the results, the authors calculated a highest predictive level (a combination of optimal sensitivity (true positive rate) and specificity (true negative rate)) of serum EPA+DHA level in calculating ST-segment re-elevation of 157 microgram/ml. For reperfusion arrhythmias, 135 microgram/ml had the highest predictive value. 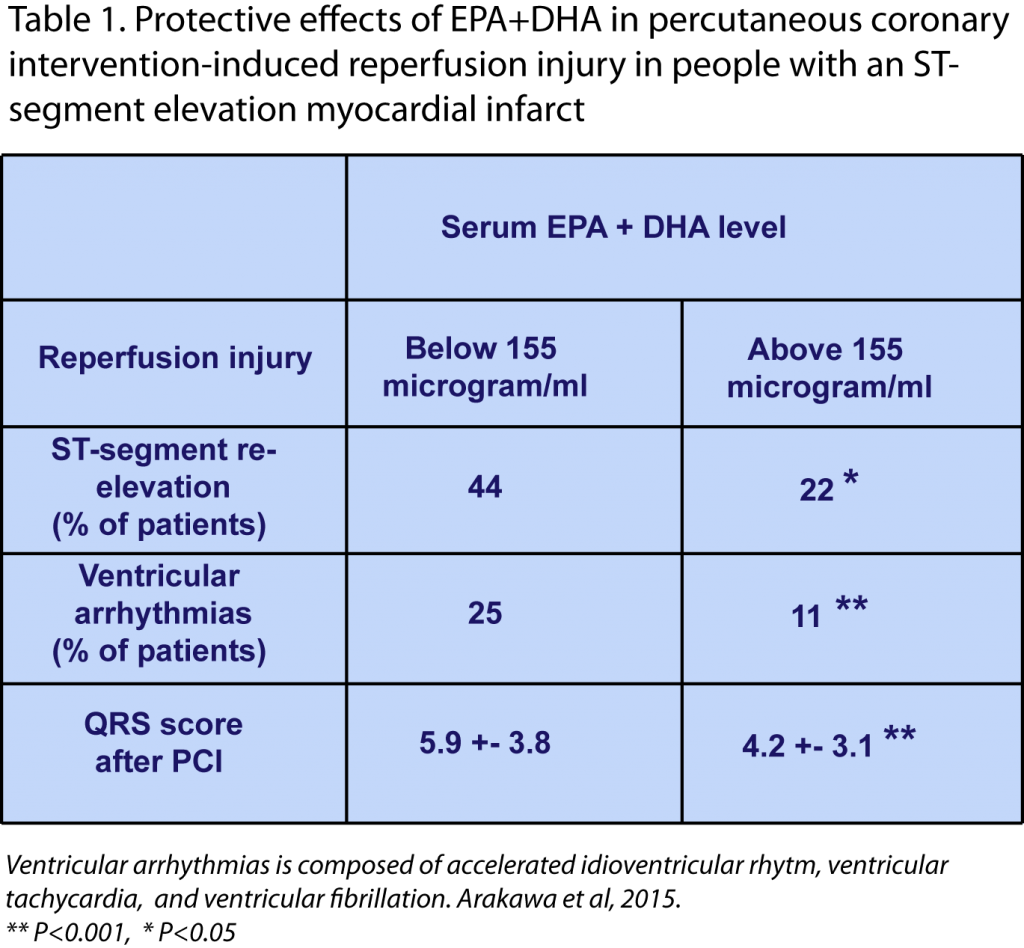 In summary, this study provides interesting new indications that in people with an acute myocardial infarction (STEMI type) and that are treated with PCI reperfusion therapy within six hours of symptoms onset, lower levels of EPA+DHA associate with a significantly increased risk of I/R injury, namely ST-segment re-elevation, reperfusion arrhythmia, and the extent of myocardial damage. The authors discuss that acute administration of omega-3 LCPUFA before or after PCI might be an adjunctive therapy to offer cardioprotection against I/R injury. This approach could be more effective in patients with a first AMI. This view is based on the fact that other studies in patients with a recurrent ventricular fibrillation have not consistently shown a measurable benefit from omega-3 LCPUFA supplementation, which the authors ascribe to concomitant therapies. The limitation of the current study is that it is an observational study, and other parameters were associated with blood levels of omega-3 LCPUFA (smoking, calcium blockers), or with a change in reperfusion injury incidence (presence of existing angina, length of ischemia). The study is of significant interest since a logical link can be postulated between the known actions of omega-3 LCPUFA and the observed protection. Confirmation of this proposed role awaits a controlled intervention trial in patients with angina that are at risk for STEMI and undergoing PCI as a preferred reperfusion treatment. Protective Actions during Myocardial Infarction The authors indicate that the mechanisms whereby omega-3 LCPUFA may reduce myocardial reperfusion injury remain to be established. A recently published study led by Ganesh Halade and colleagues at the Division of Cardiovascular Disease, Department of Medicine at the University of Alabama, Birmingham, AL, USA, has addressed how such an omega-3 LPUFA-mediated protective action may be mediated. Together with colleagues at the Center for Experimental Therapeutics and Reperfusion Injury at Brigham & Women’s Hospital, Boston, MA and the Chicago College of Pharmacy at Midwestern University, IL, the investigators examined the molecular and cellular events during ischemia-induced inflammatory damage following myocardial infarction. In a murine model of myocardial ischemia-induced infarction by permanent ligation of the left descending coronary artery, left ventricular dysfunction was induced after one to five days, as a model for ventricular remodeling and heart failure. Functional read-outs for left ventricular function were the fractional shortening (ratio between the diameter of the left ventricle when relaxed and the diameter when it is contracted), end-diastolic dimension (diameter across the left ventricle at the end of diastole), end-systolic dimension, infarcted wall thickness, and heart rate. The research addressed if the DHA-derived lipid mediator resolvin D1 (RvD1) affected ischemic ventricular remodeling and function. Results After one and five days, fractional shortening of the ventricle was markedly reduced, and ventricle diameter at systole and diastole significantly increased. The thickness of the infarcted myocardial lesion was markedly reduced. The sub-cutaneous administration of small doses of RvD1 (3 microgram/kg/day), either as the free acid or incorporated within multi-lamellar liposomes, significantly reduced the remodeling of the ventricle. RvD1 increased neutrophilic infiltration at day 1, but ablated the presence of neutrophils in the ventricle at day 5. RvD1 upregulated the expression of 5-lipoxygenase (a biosynthetic enzyme involved in wound healing and synthesis of lipid mediators), the receptor for RvD1 and lipoxin A4, an arachidonic acid-derived lipid mediator with anti-inflammatory activity. A small decrease in the number of macrophages was also induced by RvD1, and importantly the phenotype of myocardial macrophages changed from a predominant M1 classical macrophage phenotype to an M2 macrophage phenotype that play a role in resolving inflammation. Collagen deposition in the ventricle at day 5 was significantly reduced by RvD1. The functional effects of myocardial ischemia were not limited to a local response. A marked edema of the lungs appeared after one day, which was abrogated by RvD1. Following myocardial ischemia the spleen reacted rapidly with a marked reduction in weight. The involvement of the spleen, with the mobilization of pro-inflammatory leukocytes, has recently been recognized to be activated after acute myocardial infarct in humans. Also in the spleen macrophages expressed predominantly the M2 macrophage phenotype. Discussion These studies provide new insight into the potentially protective roles of omega-3 LCPUFA in the myocardium after an AMI. The studies are important since a better understanding of their role in protection from ischemia, ischemia-reperfusion injury, and incomplete reperfusion therapy, will likely help in refining interventions after acute myocardial insults. The mouse study did not address the involvement of a DHA-derived lipid mediator in reperfusion injury, but rather in a setting of prolonged ischemia-induced ventricular injury. It highlights the possibly important role of splenic activation following a myocardial infarct, and the omega-3 LCPUFA-derived lipid mediators that are formed there may play a role in activating splenic retention of immune cells that mediate ventricular damage. Further studies that directly address the relationship between blood levels or dietary intake of omega-3 LCPUFA and outcome of myocardial I/R injury and reperfusion approaches are now of significant interest and clinical value. Arakawa K, Himeno H, Kirigaya J, Otomo F, Matsushita K, Nakahashi H, Shimizu S, Nitta M, Yano H, Endo M, Kimura K, Umemura S. Impact of n-3 polyunsaturated fatty acids in predicting ischemia/reperfusion injury and progression of myocardial damage after reperfusion in patients with ST-segment elevation acute myocardial infarction. J. Cardiol. 2015;Apr. 3. [PubMed] Kain V, Ingle KA, Colas RA, Dalli J, Prabhu SD, Serhan CN, Joshi M, Halade GV. Resolvin D1 activates the inflammation resolving response at splenic and ventricular site following myocardial infarction leading to improved ventricular function. J. Mol. Cell. Cardiol. 2015;84:24-35. [PubMed] Worth Noting Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation 2013;127(24):2452-2457. [PubMed] Claeys MJ, Bosmans J, De Ceuninck M, Beunis A, Vergauwen W, Vorlat A, Vrints CJ. Effect of intracoronary adenosine infusion during coronary intervention on myocardial reperfusion injury in patients with acute myocardial infarction. Am. J. Cardiol. 2004;94(1):9-13. [PubMed] Emami H, Singh P, MacNabb M, Vucic E, Lavender Z, Rudd JH, Fayad ZA, Lehrer-Graiwer J, Korsgren M, Figueroa AL, Fredrickson J, Rubin B, Hoffmann U, Truong QA, Min JK, Baruch A, Nasir K, Nahrendorf M, Tawakol A. Splenic metabolic activity predicts risk of future cardiovascular events: demonstration of a cardiosplenic axis in humans. J.A.C.C. Cardiovasc. Imaging 2015;8(2):121-130. [PubMed] Fröhlich GM, Meier P, White SK, Yellon DM, Hausenloy DJ. Myocardial reperfusion injury: looking beyond primary PCI. Eur. Heart J. 2013;34(23):1714-1722. [PubMed] Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van De Werf F, Braunwald E. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101(2):125-130. [PubMed] James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br. J. Nutr. 2014;112(5):812-820. [PubMed] Kapela A, Bezerianos A. A theoretical model of the high-frequency arrhythmogenic depolarization signal following myocardial infarction. IEEE Trans. Biomed. Eng. 2004;51(11):1915-1922. [PubMed] van Lavieren MA, van de Hoef TP, Piek JJ. Primary PCI: time to change focus from epicardial reperfusion towards protection of the microvasculature. EuroIntervention 2014;10 (Suppl T):T39-46. [PubMed] Loring Z, Chelliah S, Selvester RH, Wagner G, Strauss DG. A detailed guide for quantification of myocardial scar with the Selvester QRS score in the presence of electrocardiogram confounders. J. Electrocardiol. 2011;44(5):544-554. [PubMed] McLennan PL. Myocardial membrane fatty acids and the antiarrhythmic actions of dietary fish oil in animal models. Lipids 2001;36 Suppl.:S111-114. [PubMed] Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD, Cleland LG. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am. J. Clin. Nutr. 2007;85(5):1222-1228. [PubMed] Mori TA. Omega-3 fatty acids and cardiovascular disease: epidemiology and effects on cardiometabolic risk factors. Food Funct. 2014;5(9):2004-2019. [PubMed] Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 Global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014;174(2):293-298. [PubMed] von Schacky C. Cardiovascular disease prevention and treatment. Prostaglandins Leukot. Essent. Fatty Acids 2009;81(2-3):193-198. [PubMed] Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U, European Association for Percutaneous Cardiovascular I. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur. Heart J. 2010;31(8):943-957. [PubMed] TIMI : TIMI Study Group http://www.timi.org/ Visual Sonics – In vivo imaging system : http://www.visualsonics.com/
In summary, this study provides interesting new indications that in people with an acute myocardial infarction (STEMI type) and that are treated with PCI reperfusion therapy within six hours of symptoms onset, lower levels of EPA+DHA associate with a significantly increased risk of I/R injury, namely ST-segment re-elevation, reperfusion arrhythmia, and the extent of myocardial damage. The authors discuss that acute administration of omega-3 LCPUFA before or after PCI might be an adjunctive therapy to offer cardioprotection against I/R injury. This approach could be more effective in patients with a first AMI. This view is based on the fact that other studies in patients with a recurrent ventricular fibrillation have not consistently shown a measurable benefit from omega-3 LCPUFA supplementation, which the authors ascribe to concomitant therapies. The limitation of the current study is that it is an observational study, and other parameters were associated with blood levels of omega-3 LCPUFA (smoking, calcium blockers), or with a change in reperfusion injury incidence (presence of existing angina, length of ischemia). The study is of significant interest since a logical link can be postulated between the known actions of omega-3 LCPUFA and the observed protection. Confirmation of this proposed role awaits a controlled intervention trial in patients with angina that are at risk for STEMI and undergoing PCI as a preferred reperfusion treatment. Protective Actions during Myocardial Infarction The authors indicate that the mechanisms whereby omega-3 LCPUFA may reduce myocardial reperfusion injury remain to be established. A recently published study led by Ganesh Halade and colleagues at the Division of Cardiovascular Disease, Department of Medicine at the University of Alabama, Birmingham, AL, USA, has addressed how such an omega-3 LPUFA-mediated protective action may be mediated. Together with colleagues at the Center for Experimental Therapeutics and Reperfusion Injury at Brigham & Women’s Hospital, Boston, MA and the Chicago College of Pharmacy at Midwestern University, IL, the investigators examined the molecular and cellular events during ischemia-induced inflammatory damage following myocardial infarction. In a murine model of myocardial ischemia-induced infarction by permanent ligation of the left descending coronary artery, left ventricular dysfunction was induced after one to five days, as a model for ventricular remodeling and heart failure. Functional read-outs for left ventricular function were the fractional shortening (ratio between the diameter of the left ventricle when relaxed and the diameter when it is contracted), end-diastolic dimension (diameter across the left ventricle at the end of diastole), end-systolic dimension, infarcted wall thickness, and heart rate. The research addressed if the DHA-derived lipid mediator resolvin D1 (RvD1) affected ischemic ventricular remodeling and function. Results After one and five days, fractional shortening of the ventricle was markedly reduced, and ventricle diameter at systole and diastole significantly increased. The thickness of the infarcted myocardial lesion was markedly reduced. The sub-cutaneous administration of small doses of RvD1 (3 microgram/kg/day), either as the free acid or incorporated within multi-lamellar liposomes, significantly reduced the remodeling of the ventricle. RvD1 increased neutrophilic infiltration at day 1, but ablated the presence of neutrophils in the ventricle at day 5. RvD1 upregulated the expression of 5-lipoxygenase (a biosynthetic enzyme involved in wound healing and synthesis of lipid mediators), the receptor for RvD1 and lipoxin A4, an arachidonic acid-derived lipid mediator with anti-inflammatory activity. A small decrease in the number of macrophages was also induced by RvD1, and importantly the phenotype of myocardial macrophages changed from a predominant M1 classical macrophage phenotype to an M2 macrophage phenotype that play a role in resolving inflammation. Collagen deposition in the ventricle at day 5 was significantly reduced by RvD1. The functional effects of myocardial ischemia were not limited to a local response. A marked edema of the lungs appeared after one day, which was abrogated by RvD1. Following myocardial ischemia the spleen reacted rapidly with a marked reduction in weight. The involvement of the spleen, with the mobilization of pro-inflammatory leukocytes, has recently been recognized to be activated after acute myocardial infarct in humans. Also in the spleen macrophages expressed predominantly the M2 macrophage phenotype. Discussion These studies provide new insight into the potentially protective roles of omega-3 LCPUFA in the myocardium after an AMI. The studies are important since a better understanding of their role in protection from ischemia, ischemia-reperfusion injury, and incomplete reperfusion therapy, will likely help in refining interventions after acute myocardial insults. The mouse study did not address the involvement of a DHA-derived lipid mediator in reperfusion injury, but rather in a setting of prolonged ischemia-induced ventricular injury. It highlights the possibly important role of splenic activation following a myocardial infarct, and the omega-3 LCPUFA-derived lipid mediators that are formed there may play a role in activating splenic retention of immune cells that mediate ventricular damage. Further studies that directly address the relationship between blood levels or dietary intake of omega-3 LCPUFA and outcome of myocardial I/R injury and reperfusion approaches are now of significant interest and clinical value. Arakawa K, Himeno H, Kirigaya J, Otomo F, Matsushita K, Nakahashi H, Shimizu S, Nitta M, Yano H, Endo M, Kimura K, Umemura S. Impact of n-3 polyunsaturated fatty acids in predicting ischemia/reperfusion injury and progression of myocardial damage after reperfusion in patients with ST-segment elevation acute myocardial infarction. J. Cardiol. 2015;Apr. 3. [PubMed] Kain V, Ingle KA, Colas RA, Dalli J, Prabhu SD, Serhan CN, Joshi M, Halade GV. Resolvin D1 activates the inflammation resolving response at splenic and ventricular site following myocardial infarction leading to improved ventricular function. J. Mol. Cell. Cardiol. 2015;84:24-35. [PubMed] Worth Noting Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation 2013;127(24):2452-2457. [PubMed] Claeys MJ, Bosmans J, De Ceuninck M, Beunis A, Vergauwen W, Vorlat A, Vrints CJ. Effect of intracoronary adenosine infusion during coronary intervention on myocardial reperfusion injury in patients with acute myocardial infarction. Am. J. Cardiol. 2004;94(1):9-13. [PubMed] Emami H, Singh P, MacNabb M, Vucic E, Lavender Z, Rudd JH, Fayad ZA, Lehrer-Graiwer J, Korsgren M, Figueroa AL, Fredrickson J, Rubin B, Hoffmann U, Truong QA, Min JK, Baruch A, Nasir K, Nahrendorf M, Tawakol A. Splenic metabolic activity predicts risk of future cardiovascular events: demonstration of a cardiosplenic axis in humans. J.A.C.C. Cardiovasc. Imaging 2015;8(2):121-130. [PubMed] Fröhlich GM, Meier P, White SK, Yellon DM, Hausenloy DJ. Myocardial reperfusion injury: looking beyond primary PCI. Eur. Heart J. 2013;34(23):1714-1722. [PubMed] Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van De Werf F, Braunwald E. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101(2):125-130. [PubMed] James MJ, Sullivan TR, Metcalf RG, Cleland LG. Pitfalls in the use of randomised controlled trials for fish oil studies with cardiac patients. Br. J. Nutr. 2014;112(5):812-820. [PubMed] Kapela A, Bezerianos A. A theoretical model of the high-frequency arrhythmogenic depolarization signal following myocardial infarction. IEEE Trans. Biomed. Eng. 2004;51(11):1915-1922. [PubMed] van Lavieren MA, van de Hoef TP, Piek JJ. Primary PCI: time to change focus from epicardial reperfusion towards protection of the microvasculature. EuroIntervention 2014;10 (Suppl T):T39-46. [PubMed] Loring Z, Chelliah S, Selvester RH, Wagner G, Strauss DG. A detailed guide for quantification of myocardial scar with the Selvester QRS score in the presence of electrocardiogram confounders. J. Electrocardiol. 2011;44(5):544-554. [PubMed] McLennan PL. Myocardial membrane fatty acids and the antiarrhythmic actions of dietary fish oil in animal models. Lipids 2001;36 Suppl.:S111-114. [PubMed] Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD, Cleland LG. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am. J. Clin. Nutr. 2007;85(5):1222-1228. [PubMed] Mori TA. Omega-3 fatty acids and cardiovascular disease: epidemiology and effects on cardiometabolic risk factors. Food Funct. 2014;5(9):2004-2019. [PubMed] Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 Global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014;174(2):293-298. [PubMed] von Schacky C. Cardiovascular disease prevention and treatment. Prostaglandins Leukot. Essent. Fatty Acids 2009;81(2-3):193-198. [PubMed] Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U, European Association for Percutaneous Cardiovascular I. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur. Heart J. 2010;31(8):943-957. [PubMed] TIMI : TIMI Study Group http://www.timi.org/ Visual Sonics – In vivo imaging system : http://www.visualsonics.com/

