Much is known about the pathology of Alzheimer’s disease, the most common form of dementia in older adults, but little is clear about what triggers the condition and how it develops. Why do some people develop the disease and others do not? Diagnosis is only known with certainty from postmortem analysis. A range of physical, neurological, laboratory, neuroimaging and psychological evaluations form the basis of a clinical diagnosis, but
onset of the disease is believed to begin 20 to 30 years before the first clinical symptoms. New
criteria for the diagnosis of Alzheimer’s disease and all-cause dementia were proposed by the U.S. National Institute on Aging in 2011. These guidelines recognize 3 stages of the disease: preclinical Alzheimer’s disease, reflecting measurable changes in the brain, cerebrospinal fluid or blood, mild cognitive impairment (MCI) due to Alzheimer’s disease and dementia due to Alzheimer’s disease. The preclinical stage is identified by biomarkers in blood or cerebrospinal fluid reflecting beta-amyloid accumulation in the brain. Symptoms of MCI, often marked by impaired episodic memory or thinking, may be noticed by the affected individual or family members and friends.
More than half of MCI patients progress to Alzheimer’s disease within 5 years. Why do some people with mildly impaired cognition progress to Alzheimer’s dementia and others remain stable?
Investigators are actively expanding the use of
biomarkers,
neuroimaging and improved
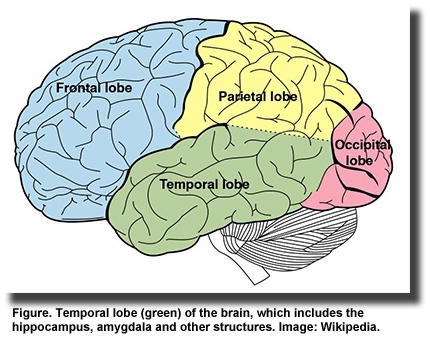
screening methods for predicting Alzheimer’s disease in cognitively normal individuals and those with MCI. It would be particularly useful to distinguish between patients with MCI who are likely to progress to Alzheimer’s disease and those who are most likely to remain cognitively stable. Changes in brain structure occur early in the disease, with atrophy of the medial temporal lobe among the first changes. Atrophy of the medial and lateral temporal lobe areas is strongly associated with
decline in memory, while advanced atrophy of cortical gray matter is associated with loss of executive function in patients with MCI and Alzheimer’s disease.
Cortical thinning in the frontal, parietal, medial temporal and occipital areas has been reported in older participants with memory decline. Others have also reported a
strong relationship between brain structural changes and cognitive function, and conversion from MCI to Alzheimer’s disease.
Another potential biomarker of Alzheimer’s disease risk may be red blood cell EPA + DHA concentration. Changes or decreases in long-chain omega-3 PUFAs (n-3 LC-PUFAs) in
plasma,
red blood cells and
brain have been associated with Alzheimer’s disease, but these relationships appear complex. It would be useful to know whether changes in plasma or red blood cell EPA + DHA were related to structural changes in brain in older adults who are at risk of MCI and Alzheimer’s disease. This question was addressed by Cecilia Samieri and colleagues at the Institut National de la Santé et de la Recherche Médicale (INSERM) in Bordeaux, France, and the Université de Sherbrooke, Canada, in a study of 72-year-old community-dwelling adults in Bordeaux. Participants with normal cognition scores (mean MMSE score = 27.9) were selected from Bordeaux, one of 3 cities involved in a prospective study of vascular risk factors for dementia. Of the 2,104 study participants, 1,419 had plasma fatty acid measurements at baseline and 504 underwent a brain magnetic resonance imaging (MRI) examination. After 4 years, 315 participants took a second MRI evaluation. After exclusions for unusable scans and missing data, 281 participants remained. The brain scans were segmented into gray and white matter and cerebrospinal fluid images, which were then used to determine whole brain and medial temporal lobe volumes. Three structures in the medial temporal lobe were selected for macroscopic neuroanatomic evaluation. Cognition was assessed using the Mini-Mental State Examination (MMSE) and the
Isaacs Set Test for verbal fluency. The investigators used the Center for Epidemiologic Studies-Depression (CES-D) scale to measure depressive symptoms.
Over the 4-year period, gray matter atrophied in the whole brain at a rate of -0.2% per year. Rates of atrophy greater than the mean were observed in the hippocampus, parahippocampus and amygdala and ranged from a rate of -0.5% per year in the left amygdala to as much as -1.0% per year in the left hippocampus. Higher baseline plasma EPA, but no other PUFA, was significantly associated with less gray matter atrophy in a region comprising 53% right amygdala, 41% right parahippocampus and 6% right hippocampus.
For distinct regions, higher plasma EPA was associated with less gray matter atrophy of the right amygdala over 4 years, but not with changes in the other medial temporal lobe areas. The association was significant after adjusting for 15 covariates and their interactions with time (
P = 0.01). Greater four-year atrophy of the right amygdala was also significantly associated with higher CES-D scores over time. Atrophy in the left amygdala was associated with a greater decline in the MMSE scores, while atrophy in both left and right amygdala correlated with a greater decline in the Isaacs Set Test scores.
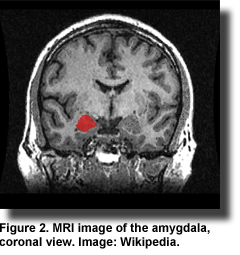
Several findings stand out. First, atrophy of gray matter in the amygdala and parts of the hippocampal area was significantly associated with plasma EPA, but not DHA, levels. Neither plasma EPA nor DHA concentrations were associated with changes in whole brain gray matter atrophy. The observation on whole brain gray matter volume supports
other similar reports. Second, only gray matter atrophy of the right amygdala, but not other medial temporal lobe regions was associated with plasma EPA concentrations.
Another study also reported an association between higher dietary EPA and DHA intake and greater gray matter volume in the right amygdala and other medial temporal lobe areas in healthy adults. Smaller brain volumes, but greater white matter hyperintensity volumes, were associated with lower red blood cell DHA levels in dementia-free adults in the
Framingham Study. Third, gray matter loss in the right and left amygdala was associated with a
decline in the Isaacs Set Test scores, a clinical assessment reflective of
early cognitive decline years before the onset of Alzheimer’s dementia. MRI-assessed atrophy in medial temporal lobe regions has been used to measure the
rate of neurodegeneration in patients with MCI, Alzheimer’s disease and healthy controls. The greatest rate of neurodegeneration occurred in the Alzheimer’s patients. Fourth, greater atrophy of the right amygdala was associated with higher depressive scores. This finding supports the results of a meta-analysis of changes in amygdala volume in major depressive disorder. That analysis reported
decreased amygdala volume in unmedicated depressed patients. Patients with depressive symptoms were reported to have
altered right amygdala responses to masked facial expressions compared with healthy controls. In the present study, plasma EPA levels were not associated with higher CES-D scores, but
previous results from this study reported an inverse relationship between plasma EPA and the severity of depressive symptoms and a
lower risk of dementia. This study provides an important link in the use of MRI to assess specific brain changes in early cognitive decline that could have implications for clinical treatments before the onset of dementia becomes irreversible. Its findings suggest that plasma EPA levels might be an important biomarker for risk of cognitive decline as well as depressive illness. Much study of the brain, cognitive function and mental illness has focused on DHA, but findings from the French Three-City study suggest that EPA bears watching as well. Samieri C, Maillard P, Crivello F, Proust-Lima C, Peuchant E, Helmer C, Amieva H, Allard M, Dartigues JF, Cunnane SC, Mazoyer BM, Barberger-Gateau P. Plasma long-chain omega-3 fatty acids and atrophy of the medial temporal lobe.
Neurology 2012;79:642-650
. [
PubMed]
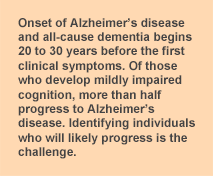 Much is known about the pathology of Alzheimer’s disease, the most common form of dementia in older adults, but little is clear about what triggers the condition and how it develops. Why do some people develop the disease and others do not? Diagnosis is only known with certainty from postmortem analysis. A range of physical, neurological, laboratory, neuroimaging and psychological evaluations form the basis of a clinical diagnosis, but onset of the disease is believed to begin 20 to 30 years before the first clinical symptoms. New criteria for the diagnosis of Alzheimer’s disease and all-cause dementia were proposed by the U.S. National Institute on Aging in 2011. These guidelines recognize 3 stages of the disease: preclinical Alzheimer’s disease, reflecting measurable changes in the brain, cerebrospinal fluid or blood, mild cognitive impairment (MCI) due to Alzheimer’s disease and dementia due to Alzheimer’s disease. The preclinical stage is identified by biomarkers in blood or cerebrospinal fluid reflecting beta-amyloid accumulation in the brain. Symptoms of MCI, often marked by impaired episodic memory or thinking, may be noticed by the affected individual or family members and friends. More than half of MCI patients progress to Alzheimer’s disease within 5 years. Why do some people with mildly impaired cognition progress to Alzheimer’s dementia and others remain stable?
Much is known about the pathology of Alzheimer’s disease, the most common form of dementia in older adults, but little is clear about what triggers the condition and how it develops. Why do some people develop the disease and others do not? Diagnosis is only known with certainty from postmortem analysis. A range of physical, neurological, laboratory, neuroimaging and psychological evaluations form the basis of a clinical diagnosis, but onset of the disease is believed to begin 20 to 30 years before the first clinical symptoms. New criteria for the diagnosis of Alzheimer’s disease and all-cause dementia were proposed by the U.S. National Institute on Aging in 2011. These guidelines recognize 3 stages of the disease: preclinical Alzheimer’s disease, reflecting measurable changes in the brain, cerebrospinal fluid or blood, mild cognitive impairment (MCI) due to Alzheimer’s disease and dementia due to Alzheimer’s disease. The preclinical stage is identified by biomarkers in blood or cerebrospinal fluid reflecting beta-amyloid accumulation in the brain. Symptoms of MCI, often marked by impaired episodic memory or thinking, may be noticed by the affected individual or family members and friends. More than half of MCI patients progress to Alzheimer’s disease within 5 years. Why do some people with mildly impaired cognition progress to Alzheimer’s dementia and others remain stable? 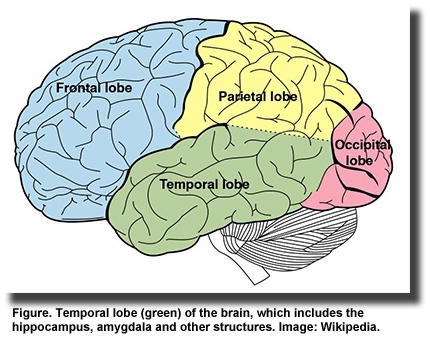 Investigators are actively expanding the use of biomarkers, neuroimaging and improved screening methods for predicting Alzheimer’s disease in cognitively normal individuals and those with MCI. It would be particularly useful to distinguish between patients with MCI who are likely to progress to Alzheimer’s disease and those who are most likely to remain cognitively stable. Changes in brain structure occur early in the disease, with atrophy of the medial temporal lobe among the first changes. Atrophy of the medial and lateral temporal lobe areas is strongly associated with decline in memory, while advanced atrophy of cortical gray matter is associated with loss of executive function in patients with MCI and Alzheimer’s disease. Cortical thinning in the frontal, parietal, medial temporal and occipital areas has been reported in older participants with memory decline. Others have also reported a strong relationship between brain structural changes and cognitive function, and conversion from MCI to Alzheimer’s disease.
Investigators are actively expanding the use of biomarkers, neuroimaging and improved screening methods for predicting Alzheimer’s disease in cognitively normal individuals and those with MCI. It would be particularly useful to distinguish between patients with MCI who are likely to progress to Alzheimer’s disease and those who are most likely to remain cognitively stable. Changes in brain structure occur early in the disease, with atrophy of the medial temporal lobe among the first changes. Atrophy of the medial and lateral temporal lobe areas is strongly associated with decline in memory, while advanced atrophy of cortical gray matter is associated with loss of executive function in patients with MCI and Alzheimer’s disease. Cortical thinning in the frontal, parietal, medial temporal and occipital areas has been reported in older participants with memory decline. Others have also reported a strong relationship between brain structural changes and cognitive function, and conversion from MCI to Alzheimer’s disease.  Another potential biomarker of Alzheimer’s disease risk may be red blood cell EPA + DHA concentration. Changes or decreases in long-chain omega-3 PUFAs (n-3 LC-PUFAs) in plasma, red blood cells and brain have been associated with Alzheimer’s disease, but these relationships appear complex. It would be useful to know whether changes in plasma or red blood cell EPA + DHA were related to structural changes in brain in older adults who are at risk of MCI and Alzheimer’s disease. This question was addressed by Cecilia Samieri and colleagues at the Institut National de la Santé et de la Recherche Médicale (INSERM) in Bordeaux, France, and the Université de Sherbrooke, Canada, in a study of 72-year-old community-dwelling adults in Bordeaux. Participants with normal cognition scores (mean MMSE score = 27.9) were selected from Bordeaux, one of 3 cities involved in a prospective study of vascular risk factors for dementia. Of the 2,104 study participants, 1,419 had plasma fatty acid measurements at baseline and 504 underwent a brain magnetic resonance imaging (MRI) examination. After 4 years, 315 participants took a second MRI evaluation. After exclusions for unusable scans and missing data, 281 participants remained. The brain scans were segmented into gray and white matter and cerebrospinal fluid images, which were then used to determine whole brain and medial temporal lobe volumes. Three structures in the medial temporal lobe were selected for macroscopic neuroanatomic evaluation. Cognition was assessed using the Mini-Mental State Examination (MMSE) and the Isaacs Set Test for verbal fluency. The investigators used the Center for Epidemiologic Studies-Depression (CES-D) scale to measure depressive symptoms. Over the 4-year period, gray matter atrophied in the whole brain at a rate of -0.2% per year. Rates of atrophy greater than the mean were observed in the hippocampus, parahippocampus and amygdala and ranged from a rate of -0.5% per year in the left amygdala to as much as -1.0% per year in the left hippocampus. Higher baseline plasma EPA, but no other PUFA, was significantly associated with less gray matter atrophy in a region comprising 53% right amygdala, 41% right parahippocampus and 6% right hippocampus.
Another potential biomarker of Alzheimer’s disease risk may be red blood cell EPA + DHA concentration. Changes or decreases in long-chain omega-3 PUFAs (n-3 LC-PUFAs) in plasma, red blood cells and brain have been associated with Alzheimer’s disease, but these relationships appear complex. It would be useful to know whether changes in plasma or red blood cell EPA + DHA were related to structural changes in brain in older adults who are at risk of MCI and Alzheimer’s disease. This question was addressed by Cecilia Samieri and colleagues at the Institut National de la Santé et de la Recherche Médicale (INSERM) in Bordeaux, France, and the Université de Sherbrooke, Canada, in a study of 72-year-old community-dwelling adults in Bordeaux. Participants with normal cognition scores (mean MMSE score = 27.9) were selected from Bordeaux, one of 3 cities involved in a prospective study of vascular risk factors for dementia. Of the 2,104 study participants, 1,419 had plasma fatty acid measurements at baseline and 504 underwent a brain magnetic resonance imaging (MRI) examination. After 4 years, 315 participants took a second MRI evaluation. After exclusions for unusable scans and missing data, 281 participants remained. The brain scans were segmented into gray and white matter and cerebrospinal fluid images, which were then used to determine whole brain and medial temporal lobe volumes. Three structures in the medial temporal lobe were selected for macroscopic neuroanatomic evaluation. Cognition was assessed using the Mini-Mental State Examination (MMSE) and the Isaacs Set Test for verbal fluency. The investigators used the Center for Epidemiologic Studies-Depression (CES-D) scale to measure depressive symptoms. Over the 4-year period, gray matter atrophied in the whole brain at a rate of -0.2% per year. Rates of atrophy greater than the mean were observed in the hippocampus, parahippocampus and amygdala and ranged from a rate of -0.5% per year in the left amygdala to as much as -1.0% per year in the left hippocampus. Higher baseline plasma EPA, but no other PUFA, was significantly associated with less gray matter atrophy in a region comprising 53% right amygdala, 41% right parahippocampus and 6% right hippocampus.  For distinct regions, higher plasma EPA was associated with less gray matter atrophy of the right amygdala over 4 years, but not with changes in the other medial temporal lobe areas. The association was significant after adjusting for 15 covariates and their interactions with time (P = 0.01). Greater four-year atrophy of the right amygdala was also significantly associated with higher CES-D scores over time. Atrophy in the left amygdala was associated with a greater decline in the MMSE scores, while atrophy in both left and right amygdala correlated with a greater decline in the Isaacs Set Test scores.
For distinct regions, higher plasma EPA was associated with less gray matter atrophy of the right amygdala over 4 years, but not with changes in the other medial temporal lobe areas. The association was significant after adjusting for 15 covariates and their interactions with time (P = 0.01). Greater four-year atrophy of the right amygdala was also significantly associated with higher CES-D scores over time. Atrophy in the left amygdala was associated with a greater decline in the MMSE scores, while atrophy in both left and right amygdala correlated with a greater decline in the Isaacs Set Test scores. 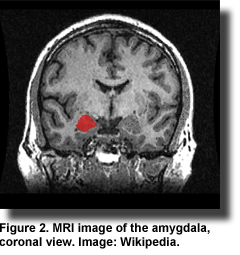 Several findings stand out. First, atrophy of gray matter in the amygdala and parts of the hippocampal area was significantly associated with plasma EPA, but not DHA, levels. Neither plasma EPA nor DHA concentrations were associated with changes in whole brain gray matter atrophy. The observation on whole brain gray matter volume supports other similar reports. Second, only gray matter atrophy of the right amygdala, but not other medial temporal lobe regions was associated with plasma EPA concentrations. Another study also reported an association between higher dietary EPA and DHA intake and greater gray matter volume in the right amygdala and other medial temporal lobe areas in healthy adults. Smaller brain volumes, but greater white matter hyperintensity volumes, were associated with lower red blood cell DHA levels in dementia-free adults in the Framingham Study. Third, gray matter loss in the right and left amygdala was associated with a
Several findings stand out. First, atrophy of gray matter in the amygdala and parts of the hippocampal area was significantly associated with plasma EPA, but not DHA, levels. Neither plasma EPA nor DHA concentrations were associated with changes in whole brain gray matter atrophy. The observation on whole brain gray matter volume supports other similar reports. Second, only gray matter atrophy of the right amygdala, but not other medial temporal lobe regions was associated with plasma EPA concentrations. Another study also reported an association between higher dietary EPA and DHA intake and greater gray matter volume in the right amygdala and other medial temporal lobe areas in healthy adults. Smaller brain volumes, but greater white matter hyperintensity volumes, were associated with lower red blood cell DHA levels in dementia-free adults in the Framingham Study. Third, gray matter loss in the right and left amygdala was associated with a  decline in the Isaacs Set Test scores, a clinical assessment reflective of early cognitive decline years before the onset of Alzheimer’s dementia. MRI-assessed atrophy in medial temporal lobe regions has been used to measure the rate of neurodegeneration in patients with MCI, Alzheimer’s disease and healthy controls. The greatest rate of neurodegeneration occurred in the Alzheimer’s patients. Fourth, greater atrophy of the right amygdala was associated with higher depressive scores. This finding supports the results of a meta-analysis of changes in amygdala volume in major depressive disorder. That analysis reported decreased amygdala volume in unmedicated depressed patients. Patients with depressive symptoms were reported to have altered right amygdala responses to masked facial expressions compared with healthy controls. In the present study, plasma EPA levels were not associated with higher CES-D scores, but previous results from this study reported an inverse relationship between plasma EPA and the severity of depressive symptoms and a lower risk of dementia. This study provides an important link in the use of MRI to assess specific brain changes in early cognitive decline that could have implications for clinical treatments before the onset of dementia becomes irreversible. Its findings suggest that plasma EPA levels might be an important biomarker for risk of cognitive decline as well as depressive illness. Much study of the brain, cognitive function and mental illness has focused on DHA, but findings from the French Three-City study suggest that EPA bears watching as well. Samieri C, Maillard P, Crivello F, Proust-Lima C, Peuchant E, Helmer C, Amieva H, Allard M, Dartigues JF, Cunnane SC, Mazoyer BM, Barberger-Gateau P. Plasma long-chain omega-3 fatty acids and atrophy of the medial temporal lobe. Neurology 2012;79:642-650. [PubMed]
decline in the Isaacs Set Test scores, a clinical assessment reflective of early cognitive decline years before the onset of Alzheimer’s dementia. MRI-assessed atrophy in medial temporal lobe regions has been used to measure the rate of neurodegeneration in patients with MCI, Alzheimer’s disease and healthy controls. The greatest rate of neurodegeneration occurred in the Alzheimer’s patients. Fourth, greater atrophy of the right amygdala was associated with higher depressive scores. This finding supports the results of a meta-analysis of changes in amygdala volume in major depressive disorder. That analysis reported decreased amygdala volume in unmedicated depressed patients. Patients with depressive symptoms were reported to have altered right amygdala responses to masked facial expressions compared with healthy controls. In the present study, plasma EPA levels were not associated with higher CES-D scores, but previous results from this study reported an inverse relationship between plasma EPA and the severity of depressive symptoms and a lower risk of dementia. This study provides an important link in the use of MRI to assess specific brain changes in early cognitive decline that could have implications for clinical treatments before the onset of dementia becomes irreversible. Its findings suggest that plasma EPA levels might be an important biomarker for risk of cognitive decline as well as depressive illness. Much study of the brain, cognitive function and mental illness has focused on DHA, but findings from the French Three-City study suggest that EPA bears watching as well. Samieri C, Maillard P, Crivello F, Proust-Lima C, Peuchant E, Helmer C, Amieva H, Allard M, Dartigues JF, Cunnane SC, Mazoyer BM, Barberger-Gateau P. Plasma long-chain omega-3 fatty acids and atrophy of the medial temporal lobe. Neurology 2012;79:642-650. [PubMed]

